3709
Comparison of Multiplexed Sensitivity Encoding and Reduced Field-of-view Technique for Diffusion-Weighted Imaging of the Prostate1Department of Diagnostic and Interventional Radiology, Osaka University Graduate School of Medicine, Suita, Japan
Synopsis
The image quality and diagnostic performance of diffusion weighted imaging (DWI) using multiplexed sensitivity encoding (MUSE) and DWI using reduced field-of-view (rFOV) technique in detecting prostate cancer were compared. Visual scores of MUSE-DWI regarding the visibility of prostate anatomy and overall image quality were significantly higher than those of rFOV-DWI. The diagnostic performance in detecting prostate cancer was not significantly different between MUSE-DWI and rFOV-DWI. MUSE yielded high quality DWI without reducing FOV and is expected to be more useful than rFOV technique for evaluation of the prostate including lymph node metastasis.
Introduction
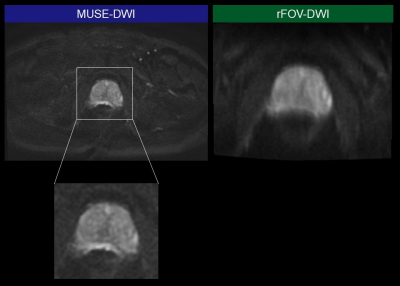
Diffusion-weighted imaging (DWI) is an essential imaging technique for the detection of prostate cancer, and is especially useful for peripheral zone cancer1. DWI with higher spatial resolution would improve the detectability of small tumors. Reduced field-of-view (rFOV) DWI is a promising technique which enables higher spatial resolution imaging2, 3. However, because of its limited FOV, it is not suitable for evaluating the entire pelvis, including lymph nodes. Recently, multiplexed sensitivity encoding (MUSE), a multi-shot segmented echo planar imaging technique, has been introduced to clinical practice4. This technique would provide higher spatial resolution DWI without reducing FOV, and allow for evaluation of both prostate and pelvic lymph nodes (Figure 1). However, the usefulness of this technique in prostate MR imaging has not been well investigated. The purpose of this study was to retrospectively compare the image quality and the diagnostic performance between MUSE-DWI and rFOV-DWI for prostate MR imaging.Methods
This study was approved by our institutional review board, and the requirement for informed consent was waived. Forty patients who were suspected of having a prostate cancer and underwent prostate MR imaging including MUSE-DWI and rFOV-DWI using a 3-Tesla scanner were enrolled in this study. Apparent diffusion coefficient (ADC) maps and computed DWI with a b value of 2000 s/mm2 were calculated using b = 0 and 1000 s/mm2 images for both MUSE-DWI and rFOV-DWI. ADC values of peripheral zone (PZ), transitional zone (TZ) were compared between MUSE-DWI and rFOV-DWI using the paired t-test. In patients with tumors, ADC values of the tumors were also compared. Two radiologists independently evaluated the image quality of b = 1000 images regarding the visibility of prostate anatomy, image noise, distortion, and overall image quality using a 5-point rating scale, and scores for MUSE-DWI and rFOV-DWI were compared using the Wilcoxon signed-rank test. They also evaluated the image set of T2-weighted images (T2WI) and MUSE-DWI (including ADC map and computed DWI), as well as the set of T2WI and rFOV-DWI, and scored the possibility of the presence of a prostate cancer using Prostate Imaging-Reporting and Data System (PI-RADS) version 2.11. The diagnostic performance was compared between two image sets using receiver operating characteristic (ROC) analysis.Results
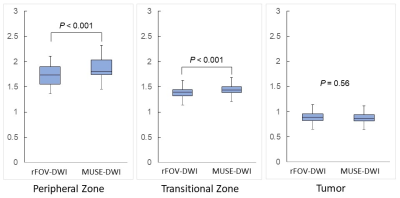
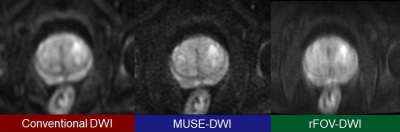
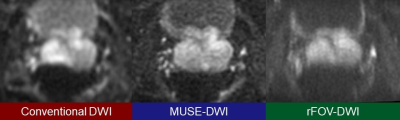
ADC values of PZ and TZ measured on MUSE-DWI were significantly higher than those on rFOV-DWI (1.85 vs 1.74 and 1.45 vs 1.39 ×10-3 mm2/s, respectively, P < .001) (Figure 2). There was no significant difference between the ADC values of tumors measured on MUSE-DWI and those on rFOV-DWI (0.88 vs 0.90 ×10-3 mm2/s, P = 0.56). Mean visual scores of MUSE-DWI were significantly higher than those of rFOV-DWI regarding the visibility of prostate anatomy and overall image quality for both readers, and regarding the image noise and distortion for one of the two readers (P < .001) (Figure 3, 4). Area under the curves for the detection of prostate cancer were not significantly different between T2WI+MUSE-DWI and T2WI+rFOV-DWI for both readers (0.69 and 0.69 for Reader 1, P = 0.96, and 0.59 and 0.71 for Reader 2, P = 0.23, respectively). The interobserver agreement of PI-RADS categories was higher for MUSE-DWI than for rFOV-DWI (weighted kappa: 0.70 vs 0.52).Discussion
ADC values were significantly different between MUSE-DWI and rFOV-DWI in PZ and TZ, while they were not significantly different in tumors. The reason for this is unclear, but the differences in values were 0.11 and 0.06 ×10-3 mm2/s for PZ and TZ, respectively, and should not be a major problem in clinical use. MUSE-DWI had significantly higher visual scores regarding the visibility of structures and overall image quality compared with rFOV-DWI. It would contribute to the depiction of prostate structures in more detail, and may helpful for the detection of smaller lesions. Moreover, MUSE-DWI had significantly higher visual scores regarding the distortion for one reader, and it may also improve lesion detectability and diagnostic confidence by providing less distorted images. There was no significant difference in diagnostic performance in detecting prostate cancer between MUSE-DWI and rFOV-DWI. Both techniques provide high-resolution DWI and are expected to be useful for detecting small cancers. However, further studies with more cases will be needed to determine if the diagnostic performance can be improved compared to conventional DWI.Conclusion
MUSE enabled prostate DWI with higher image quality and comparable diagnostic performance compared to rFOV technique. MUSE would provide high quality DWI with a wide FOV and is expected to be more useful than rFOV technique for evaluation of the prostate including lymph node metastasis.Acknowledgements
No acknowledgement found.References
1. Turkbey B, Rosenkrantz AB, Haider MA, et al. Prostate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2. Eur Urol. 2019;76(3):340-351.
2. Ota T, Hori M, Onishi H, et al. Preoperative staging of endometrial cancer using reduced field-of-view diffusion-weighted imaging: a preliminary study. Eur Radiol. 2017;27(12):5225-5235.
3. Tamada T, Ream JM, Doshi AM, Reduced Field-of-View Diffusion-Weighted Magnetic Resonance Imaging of the Prostate at 3 Tesla: Comparison With Standard Echo-Planar Imaging Technique for Image Quality and Tumor Assessment. J Comput Assist Tomogr. 2017;41(6):949-956.
4. Baxter GC, Patterson AJ, Woitek R, et al. Improving the image quality of DWI in breast cancer: comparison of multi-shot DWI using multiplexed sensitivity encoding to conventional single-shot echo-planar imaging DWI. Br J Radiol. 2021;94(1119):20200427.
Figures