3702
MRI in the differential diagnosis of angular pregnancy and interstitial pregnancy during the first trimester1Beijing Friendship Hospital Affiliated to Capital Medical University, Beijing, China, 2School of Clinical Medicine, Jining Medical University, Jining, China, 3Jining No. 1 Peoples’ Hospital, Jining, China
Synopsis
The study evaluated the accuracy of MRI in the diagnosis of 22 angular pregnancy cases and 37 interstitial pregnancy cases retrospectively during the first trimester. Two senior obstetrics radiologists reviewed the MR images and analyzed several features. The study found two key features were useful to diagnose angular pregnancy, namely, “medial free edge” and “medial free edge plus above-cutoff endometrial thickness”. One key feature to diagnose interstitial pregnancy was “intact lateral junctional zone”. MRI is a novel imaging approach to make the precise differential diagnosis of angular pregnancy and interstitial pregnancy.
INTRODUCTION
It is challenging to differentiate angular pregnancy from other ectopic pregnancies in the uterotubal junction, among which interstitial pregnancy is most common. 1, 2 It is of great importance to make a precise diagnosis of angular pregnancy and interstitial pregnancy during the first trimester, since a misdiagnosis of these two entities may result in either the termination of a viable pregnancy 2, 3 or life-threatening gynecologic emergencies 4-6.First-trimester ultrasonography is a routine imaging approach for assessing patients with suspected ectopic pregnancies. However, the unusual implantation sites of angular and interstitial pregnancies, which may also coexist with heavy hemorrhage, bowel gas, and ovarian masses, may interfere with the diagnostic accuracy of this operator-dependent imaging modality.7-9 MRI may have unique advantages for the differential diagnosis of angular pregnancy and interstitial pregnancy, which are easily misdiagnosed and confused with each other during the first trimester.3, 4
Using operative and pathological reports as the reference standard, we established a retrospective cohort of patients preoperatively diagnosed with uterotubal junctional pregnancies. We hypothesized that angular pregnancy and interstitial pregnancy can be precisely differentiated by MRI.
METHODS
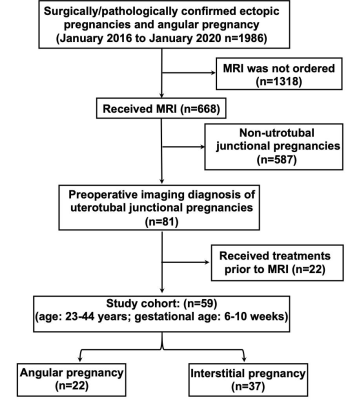
This retrospective study involved 59 patients (age: 23 - 44 years; gestational age: 6 - 10 weeks) with a preoperative imaging diagnosis of uterotubal junctional pregnancy. Using operative and pathological reports as the reference standard, 22 patients were diagnosed with angular pregnancy and 37 patients were diagnosed with interstitial pregnancy (Fig 1). Two senior obstetrics radiologists, who were blinded to the patients’ information, reviewed the MR images. Any disagreement was resolved by discussion to achieve a consensus. The sensitivity and specificity of each MRI finding were calculated in accordance with the reference standard.RESULTS
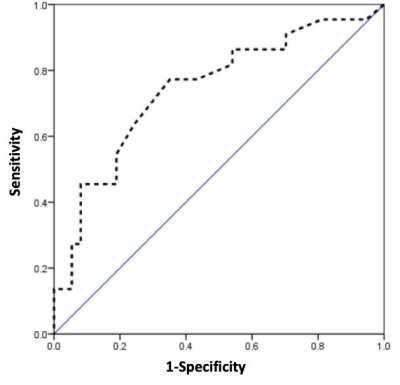
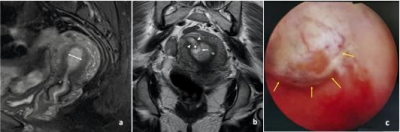
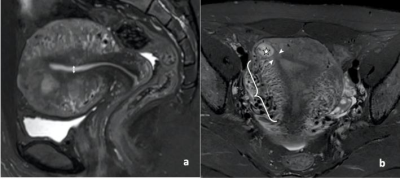
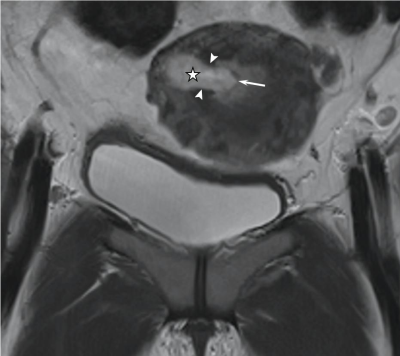
The endometrial thickness in the angular pregnancy groups was significantly larger than in the interstitial group (p = 0.001). The cutoff value of the endometrial thickness was 11.5 mm with a sensitivity, specificity, Youden’s index, and area under the curve that were 77.3%, 64.9%, 42.4%, and 0.743, respectively (Fig 2). Two key features were useful to diagnose angular pregnancy (Fig 3), namely, “medial free edge” and “medial free edge plus above-cutoff endometrial thickness”. The sensitivity and specificity of the medial free edge were 100% and 94.9%, respectively. The sensitivity and specificity of the medial free edge plus above-cutoff endometrial thickness were 77.3% and 100%, respectively. The key feature to diagnose interstitial pregnancy (Fig 4) was an “intact lateral junctional zone”, of which the sensitivity and specificity were 94.6% and 100%, respectively. Two patients with interstitial pregnancy were false-negative for this sign because the gestational sac in both patients protruded into the uterine cavity, leading to an interruption of the junctional zone ( Fig. 5).DISCUSSION
The medial free edge was a novel MRI feature to diagnose angular pregnancy. Similar to the medial free edge we demonstrated, Bradly et.al. 10 and Grant et.al. 3 identified “double sac” and “surrounding endometrium” by ultrasonography. The MRI and hysteroscopic results in our study, together with the previous ultrasonographic findings 3,10, indicate that the medial free edge is a highly sensitive feature for the diagnosis of angular pregnancy.Endometrial thickness is an independent risk factor that has been used to predict the occurrence of ectopic pregnancy.11-14 Similar to findings in previous publications 11-13,15, the endometrial thickness in the angular pregnancy group was significantly higher than in the interstitial pregnancy group, in our study. After combining the above-cutoff (11.5 mm) endometrial thickness and medial free edge, the specificity was increased to 100% since the two patients who were false positive for the medial free edge sign had an endometrial thickness that was less than 11.5mm. Given that the endometrial thickness is proportional to the pregnancy viability 12, 16 and a medial free edge indicates the eccentric, angular implantation of a gestational sac, the extremely high specificity of the combination of these two signs suggests the high concordance between MRI features and the biological characteristics of angular pregnancy, which is a potentially viable intracavitary pregnancy implanting in the uterine cornua.
While the sign of “ intact lateral junctional zone” has been previously reported 17,18,19, we further confirmed this sign not only by introducing a solid reference standard and using a larger sample size, but also by emphasizing the anatomical location that is between the uterine cavity and the external tangent gestational sac. The false-negative rate for this sign was 5.4% (2/37) since the two false-negative patients showed gestational sacs that protruded into the uterine cavity, resulting in an interrupted junctional zone. Not surprisingly, the same patients were also false positive for the sign of medial free edge.
The presence of flow-void in MRI suggests enhanced blood flow through dilated blood vessels 20,. Thus, the sign of enhanced ipsilateral flow-void in the patients with interstitial pregnancy might be owing to the ectopically implanted gestational sac that facilitates the proliferation of ipsilateral blood vessels.
CONCLUSION
MRI is a novel imaging approach that can be used to make the precise differential diagnosis of angular pregnancy and interstitial pregnancy during the first trimester.Acknowledgements
We thank the obstetrics and gynecology team of Jining No.1 People’s Hospital for collecting and providing the hysteroscopic images; and Jane Charbonneau, DVM, from Liwen Bianji (Edanz) (www.liwenbianji.cn/) for editing the English text of a draft of this manuscript.
References
1. Arleo EK, DeFilippis EM. Cornual, interstitial, and angular pregnancies: clarifying the terms and a review of the literature. Clin Imaging 2014; 38: 763-770.
2. Finlinson AR, Bollig KJ, Schust DJ. Differentiating pregnancies near the uterotubal junction (angular, cornual, and interstitial): a review and recommendations. Fertil Res Pract 2020; 6: 8.
3. Grant A, Murji A, Atri M. Can the Presence of a Surrounding Endometrium Differentiate Eccentrically Located Intrauterine Pregnancy from Interstitial Ectopic Pregnancy? J Obstet Gynaecol Can 2017; 39: 627-634.
4. Marfori CQ, Kotzen M. Angular vs. interstitial pregnancy: A case report highlighting diagnostic nuances with stark management differences. Case Rep Womens Health 2018; 19: e00068.
5. Moawad NS, Mahajan ST, Moniz MH, Taylor SE, Hurd WW. Current diagnosis and treatment of interstitial pregnancy. Am J Obstet Gynecol 2010; 202: 15-29.
6. Alalade AO, Smith FJE, Kendall CE, Odejinmi F. Evidence-based management of non-tubal ectopic pregnancies. J Obstet Gynaecol 2017; 37: 982-991.
7. Koroglu M, Kayhan A, Soylu FN, Erol B, Schmid-Tannwald C, Gurses C, Karademir I, Ernst R, Yousuf A, Oto A. MR imaging of ectopic pregnancy with an emphasis on unusual implantation sites. Jpn J Radiol 2013; 31: 75-80.
8. Kao LY, Scheinfeld MH, Chernyak V, Rozenblit AM, Oh S, Dym RJ. Beyond ultrasound: CT and MRI of ectopic pregnancy. AJR Am J Roentgenol 2014; 202: 904-911.
9. Rana P, Kazmi I, Singh R, Afzal M, Al-Abbasi FA, Aseeri A, Singh R, Khan R, Anwar F. Ectopic pregnancy: a review. Arch Gynecol Obstet 2013; 288: 747-757.
10. Bradley WG, Fiske CE, Filly RA. The double sac sign of early intrauterine pregnancy: use in exclusion of ectopic pregnancy. Radiology 1982; 143: 223-226.
11. Spandorfer SD, Barnhart KT. Endometrial stripe thickness as a predictor of ectopic pregnancy. Fertil Steril 1996; 66: 474-477.
12. Liu H, Zhang J, Wang B, Kuang Y. Effect of endometrial thickness on ectopic pregnancy in frozen embryo transfer cycles: an analysis including 17,244 pregnancy cycles. Fertil Steril 2020; 113: 131-139.
13. Levgur M, Tsai T, Kang K, Feldman J, Kory LA. Endometrial stripe thickness in tubal and intrauterine pregnancies. Fertil Steril 2000; 74: 889-891.
14. Dart RG, Dart L, Mitchell P, Berty C. The predictive value of endometrial stripe thickness in patients with suspected ectopic pregnancy who have an empty uterus at ultrasonography. Acad Emerg Med 1999; 6: 602-608.
15. Seeber B, Sammel M, Zhou L, Hummel A, Barnhart KT. Endometrial stripe thickness and pregnancy outcome in first-trimester pregnancies with bleeding, pain or both. J Reprod Med 2007; 52: 757-761.
16. Babayev E, Robins JC. Endometrial thickness as an independent risk factor for ectopic pregnancy in in vitro fertilization: should we change our counseling and practice? Fertil Steril 2020; 113: 78-79.
17. Tamai K, Koyama T, Togashi K. MR features of ectopic pregnancy. Eur Radiol 2007; 17: 3236-3246.
18. Filhastre M, Dechaud H, Lesnik A, Taourel P. Interstitial pregnancy: role of MRI. Eur Radiol 2005; 15: 93-95.
19. Choi JA, Lee KH, Jun WS, Yi MG, Lee S, Kang HS. Osseous metastasis from renal cell carcinoma: "flow-void" sign at MR imaging. Radiology 2003; 228: 629-634.
20. Murphy J, Patel A, James SL, Botchu R, Davies AM. "Flow-void" sign in osseous metastatic renal cell carcinoma. Clin Radiol 2019; 74: 111-115.
Figures