3701
Simplified VI-RADS based on biparametric MRI for the detection of muscle-invasive bladder cancer
Lei Ye1, Xiaoyong Zhang2, Yuntian Chen1, and Hui Xu1
1Department of Radiology, West China Hospital, Sichuan University, Chengdu, Sichuan, China, 2Clinical Science, Philips Healthcare, Chengdu, Sichuan, China
1Department of Radiology, West China Hospital, Sichuan University, Chengdu, Sichuan, China, 2Clinical Science, Philips Healthcare, Chengdu, Sichuan, China
Synopsis
There are different opinions about the importance of dynamic contrast enhancement (DCE) in VI-RADS among patients with bladder cancer (BCa), for the limited contribution for identifying muscle invasiveness and gadolinium-related toxicity. This study head-to-head compared the diagnostic accuracy between simplified VI-RADS excluding DCE sequence and conventional VI-RADS including DCE sequence. Our results showed that the diagnostic performance was comparable between these two MRI protocols.
Introduction
Vesical Imaging Reporting and Data System (VI-RADS) is applied to preoperatively assess the presence of muscle invasiveness of bladder cancer (MIBC).1 There are different opinions about the importance of dynamic contrast enhancement (DCE) in VI-RADS among patients with bladder cancer (BCa), and in part studies has presented that DCE sequence is of few value for the VI-RADS. 2 Moreover, there have been safety concerns related to gadolinium-based contrast agents, such as contrast allergies, gadolinium deposition in the brain, and nephrogenic systemic fibrosis in rare cases. 3 Therefore, we conducted this preliminary study to head-to-head compare the diagnostic accuracy of simplified VI-RADS without the using of DCE sequence and conventional VI-RADS in discriminating MIBC from non-muscle-invasive BCa (NMIBC).Patients and methods
This study was approved by the institutional ethics committee. A total of twenty-five patients were prospectively recruited and underwent clinically indicated multiparametric MRI (mpMRI) between May 2021 and September 2021. All patients underwent transurethral resection of bladder tumor (TURBT) or radical cystectomy (RC), and further histologically proved urothelial BCa would be finally included in the assessment.The MR examination was performed on a 3T MR scanner (Elition, Philips) equipped with a 32-channel phased array surface coil. The MR protocol included the following sequences: T2-weighted fast spin echo sequence (T2WI), diffusion-weighted imaging (DWI), and T1-weighted 3D spoiled gradient-echo DCE after Gadoteridol injection. Regarding DWI, three b-values (b=0, 800, 1000) were acquired and apparent diffusion coefficient maps (ADC maps) were calculated.
Three radiologists (2 urological radiologists with experience of 3 and 5 years respectively, and 1 expert radiologists with 15 years in abdominal radiology) interpreted the bpMRI (T2WI and DWI) and mpMRI (T2WI, DWI, and DCE) independently in two reading sessions separated by at least one month to avoid recall bias. Assessment criteria for muscle invasiveness followed VI-RADS on a 5-point scale: 1, highly likely; 2, unlikely; 3, equivocal; 4, likely; 5, very likely. VI-RADS scores of 1~2 were considered NMIBC, while 3~5 were considered MIBC, as shown in Figure 1. The reference standard was pathological result derived from primary or secondary TURBT, or RC. Sensitivity and specificity were calculated for each reader, and performance was assigned using operating characteristic (ROC) curves. All statistical analyses were performed by using IBM SPSS statistics software (IBM, version 20). A two-sided p value < 0.05 was considered statistically significant.
Results
As showed in table 1, the AUCs for bp- and mp-MRI were respectively 0.83-0.88 (reader 1), 0.88-0.84 (reader 2), 0.92-0.84 (reader 3). Sensitivity ranged between 66.7 and 83.3% and between 75.0 and 83.3% for bpMRI and mpMRI respectively, while specificity reached 85% for both protocols. There was no significant difference in diagnostic performance between these two MRI protocols (p> 0.05). Our study showed that the diagnostic specificity of mpMRI was poorer than bpMRI, though the difference was not statistically significant (p> 0.05).Discussion and Conclusion
The abbreviated MRI protocol consisting of T2WI and DWI has a comparable diagnostic performance to the conventional mpMRI protocol for the detection of MIBC. The plausible explanation for the lower specificity might be that the DCE might increase the difficulty of image interpretation of standard mpMRI.Acknowledgements
NoneReferences
1. Panebianco V, Narumi Y, Altun E, et al. Multiparametric Magnetic Resonance Imaging for Bladder Cancer: Development of VI-RADS (Vesical Imaging-Reporting And Data System). Eur Urol. 2018;74(3):294-306. doi:10.1016/j.eururo.2018.04.0292. Delli Pizzi A, Mastrodicasa D, Marchioni M, et al. Bladder cancer: do we need contrast injection for MRI assessment of muscle invasion? A prospective multi-reader VI-RADS approach. Eur Radiol. Published online November 19, 2020. doi:10.1007/s00330-020-07473-6
3. Ramalho M, Ramalho J, Burke LM, Semelka RC. Gadolinium Retention and Toxicity-An Update. Adv Chronic Kidney Dis. 2017;24(3):138-146. doi:10.1053/j.ackd.2017.03.004
Figures
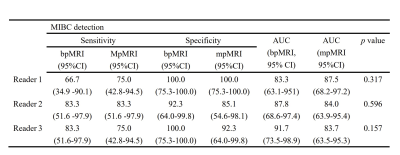
Table 1. Diagnostic performance of the three readers regarding the MIBC detection for bpMRI and mpMRI.
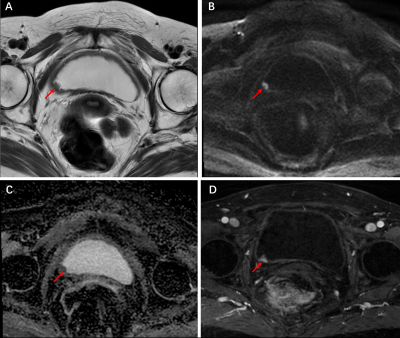
Figure 1. Images in a 70-year-old woman with pathologically proven NMIBC with inconsistent scores from bp- and mp-MRI. (A) Axial T2WI confirmed a lesion with low signal intensity on the right-posterior wall of bladder, and a score of 3 was given. (B) Axial DWI showed a high signal intensity lesion with a low-intensity stalk at b = 1000, and a score of 2 was given. (C) Calculated ADC map with b=0,1000, and the lesion was in low intensity. (D) DCE image showed tumor early enhancement extended focally to muscular layer, and a score of 4 was given. Final bpMRI score was 2, while the mpMRI score was 4.
DOI: https://doi.org/10.58530/2022/3701