3698
Diagnostic value of adding MRI to CT examination for evaluating cystic renal masses using the 2019 Bosniak classification.1Radiology, Keio University School of Medicine, Tokyo, Japan, 2Urology, Tokyo Medical and Dental University Graduate School, Tokyo, Japan, 3Radiology, University Medical Center Groningen, Groningen, Netherlands, 4Radiology, National Defence Medical College, Saitama, Japan, 5Radiation Technology, Keio University Hospital, Tokyo, Japan
Synopsis
We compared the interobserver agreement and diagnostic performance of CT alone and combined CT/MRI among two groups of readers (radiologists and residents) using the 2019 Bosniak classification (BC2019) to determine the malignancy of cystic renal masses (CRMs). Our study demonstrated that combined CT/MRI resulted in substantially high interobserver agreement between radiologists and residents. In addition, the diagnostic performance for category III/IV malignancy improved significantly for residents with combined CT/MRI when compared with evaluations based on CT alone. Thus, combined CT/MRI may be useful for diagnosing malignancy in CRMs, especially for non-expert readers, using the (BC2019).
Introduction:
The Bosniak classification (BC) was first described in 1986 for CT-based risk stratification of cystic renal masses (CRMs) according to the probability of malignancy.1 Because the original BC did not include any criterion for MRI evaluation and exhibited interobserver variability, it was updated in 2019.2-5 Compared with the 2005 version, the latest version provides better interobserver agreement by incorporating the criteria for MRI and detailing subjective evaluation criteria.6-8 Nevertheless, the value of adding MRI to CT examination (combined CT/MRI) in the 2019 Bosniak classification (BC2019) remains unknown. We compared the diagnostic performance of CT alone and combined CT/MRI using the BC2019.Methods:
This study was approved by the Institutional Review Board. As this was a retrospective study, the requirement for written informed consent was waived. In total, 103 CRMs from 83 consecutive patients assessed with both contrast-enhanced CT and MRI before surgery between 2010 and 2016 were included (Fig.1). CT images were obtained using 128-slice multi-detector row CT systems, and MRI examinations were performed using a 1.5-T MRI system with 32-channel phased-array coils (Fig.2). For image analysis, six readers in two groups (three radiologists and three radiology residents) independently reviewed CT alone and combined CT/MRI data using the BC2019. For each reader, there was at least a 1-month interval between reading pairs of images (i.e., CT alone and combined CT/MRI) to avoid recall bias. Overall, the Bosniak category was determined by consensus in each group, with Bosniak categories III/IV considered malignant. Interobserver agreement in each group was assessed using Fleiss’ kappa values. The effect of different modalities on malignancy detection was assessed using the McNemar’s test. For patients who underwent radical or partial nephrectomy, a final diagnosis was made using histopathological findings. For the remaining patients, all clinical and imaging follow-up data were used as reference standards.6, 9, 10Results:
The baseline characteristics of the patients and their renal masses are summarized in Fig.3. For CT alone/combined CT/MRI, interobserver agreement was substantial for both radiologists and residents (Fleiss κ values: 0.77/0.78 and 0.63/0.65, respectively). The number of cases changing from category I/II on CT alone to category IIF on combined CT/MRI was 8 (7.8%) for radiologists and 12 (11.7%) for residents. Furthermore, the number of cases changing from category IIF on CT alone to category III/IV on combined CT/MRI was 4 (3.9%) for radiologists and 6 (5.8%) for residents. A representative case of discordance in the categorization between CT and MRI is shown in Fig.4.The diagnostic performance of each group of readers for detecting malignancy is shown in Fig.5. Among residents, the sensitivity, specificity, and accuracy of combined CT/MRI and CT alone were respectively 82.1%, 74.7%, and 76.7% and 75.0%, 66.7%, and 68.9%, with combined CT/MRI being significantly higher than CT alone in terms of specificity and accuracy (p=0.03, and 0.008, respectively). However, the sensitivity, specificity, and accuracy for detecting malignancy did not significantly differ between combined CT/MRI and CT alone among radiologists (89.3%, 74.7%, and 78.6% vs. 85.7%, 73.3%, and 76.7%, p=0.32, 0.56, and 0.32, respectively). The proportion of CRMs whose evaluations were upgraded from category IIF to category III/IV during follow-up did not significantly differ between combined CT/MRI and CT alone according to the evaluations of the two reader groups (radiologists: 10.5% vs. 11.8%, p=0.32; residents: 10.0% vs. 9.1%, p=0.75).
Discussion:
In this study, we compared interobserver agreement for CT alone and combined CT/MRI between the two groups of readers using the BC2019 to determine the malignancy of CRMs. Our findings indicated that combined CT/MRI yielded high interobserver agreement, which was comparable among radiology residents and board-certified radiologists. Notably, radiology residents achieved a significantly higher specificity and accuracy for malignancy (when considering categories III/IV as positive) on combined CT/MRI than on CT alone. Therefore, combined CT/MRI scans may improve the diagnostic utility of the BC2019, especially for non-expert readers, such as radiology residents.This study found a high level of interobserver agreement among the different readers for the assessment of critical imaging features assessment on both CT alone and combined CT/MRI. However, certain features of CRMs remain difficult to reproducibly quantify or qualify using MRI, as reported by Edney et al..11Therefore, specifying or prioritizing the sequence (specifically T2-weighted imaging or post-contrast fat-suppressed T1-weighted imaging) for evaluating each critical imaging feature may further improve interobserver agreement for MRI assessment. However, further studies are required to confirm this hypothesis.
Limitations
First, several masses were determined as malignant using the clinical reference standard and not through surgical intervention.6, 9, 10 Second, according to the standard workup of CRMs in our hospital, both CT and MRI were performed for baseline evaluation. However, in some cases, MRI was performed for assessing CRMs after evaluation by other modalities (i.e., CT or ultrasonography), which may have introduced some selection bias.6, 7, 12, 13 Finally, this retrospective study included a small sample size. Further large-scale validation studies are required to confirm our findings.
Conclusion:
Combined CT/MRI may be useful for diagnosing malignancy in patients with CRMs using the BC2019, especially for non-expert readers.Acknowledgements
The authors thank Mr. Koshi Okabe and Ms. Sari Motomatsu for their help with data collection.References
1. Bosniak MA. The current radiological approach to renal cysts. Radiology 1986;158:1–10.
2. Israel GM, Hindman N, Bosniak MA. Evaluation of cystic renal masses: comparison of CT and MR imaging by using the Bosniak classification system. Radiology 2004;231:365–371.
3. Ferreira AM, Reis RB, Kajiwara PP, Silva GE, Elias J Jr, Muglia VF. MRI evaluation of complex renal cysts using the Bosniak classification: a comparison to CT. Abdom Radiol (NY) 2016;41:2011–2019.
4. Zhong J, Cao F, Guan X, Chen J, Ding Z, Zhang M. Renal cyst masses (Bosniak category II-III) may be over evaluated by the Bosniak criteria based on MR findings. Medicine (Baltimore) 2017;96:e9361.
5. Kim WB, Lee SW, Doo SW, et al. Category migration of renal cystic masses with use of gadolinium-enhanced magnetic resonance imaging. Korean J Urol 2012;53:573–576.
6. Silverman SG, Pedrosa I, Ellis JH, et al. Bosniak classification of cystic renal masses, version 2019: an update proposal and needs assessment. Radiology 2019;292:475–488.
7. Schieda N, Davenport MS, Krishna S, et al. Bosniak classification of cystic renal masses, version 2019: a pictorial guide to clinical use. Radiographics 2021;41:814–828.
8. Bai X, Sun SM, Xu W, et al. MRI-based Bosniak classification of cystic renal masses, version 2019: interobserver agreement, impact of readers' experience, and diagnostic performance. Radiology 2020;297:597–605.
9. Hindman NM, Hecht EM, Bosniak MA. Follow-up for Bosniak category 2F cystic renal lesions. Radiology 2014;272:757–766.
10. Chan J, Yan JH, Munir J, et al. Comparison of Bosniak classification of cystic renal masses version 2019 assessed by CT and MRI. Abdom Radiol (NY) 2021;46:5268–5276.
11. Edney E, Davenport MS, Curci N, et al. Bosniak classification of cystic renal masses, version 2019: interpretation pitfalls and recommendations to avoid misclassification. Abdom Radiol (NY). 2021;46:2699–2711.
12. Krishna S, Schieda N, Pedrosa I, et al. Update on MRI of cystic renal masses including Bosniak version 2019. J Magn Reson Imaging 2021;54:341–356.
13. Zeng SE, Du MY, Yu Y, et al. Ultrasound, CT, and MR imaging for evaluation of cystic renal masses. J Ultrasound Med 2021; Epub ahead of print. doi: 10.1002/jum.15762.
Figures
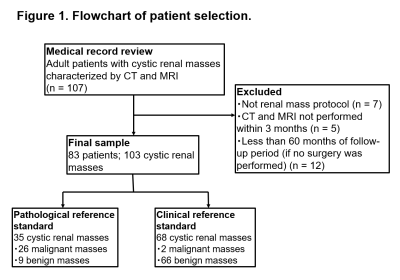
Figure 1. Flowchart of patient selection.
CT, computed tomography; MRI, magnetic resonance imaging.
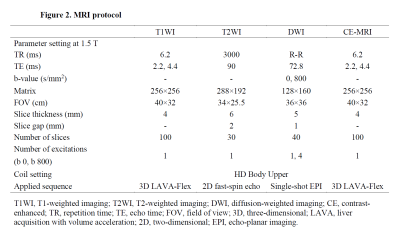
Figure 2. MRI protocol.
T1WI, T1-weighted imaging; T2WI, T2-weighted imaging; DWI, diffusion-weighted imaging; CE, contrast-enhanced; TR, repetition time; TE, echo time; FOV, field of view; 3D, three-dimensional; LAVA, liver acquisition with volume acceleration; 2D, two-dimensional; EPI, echo-planar imaging.

Figure 3. Baseline characteristics of the patients (n = 83) and renal masses (n = 103)
CT, computed tomography; MEST, mixed epithelial and stromal tumor; MCNLMP, multilocular cystic renal neoplasm of low malignant potential; MRI, magnetic resonance imaging.
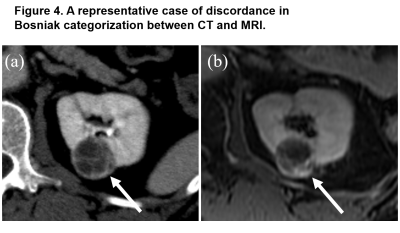
Figure 4. A representative case of discordance in Bosniak categorization between CT and MRI.
A 46-year-old woman with cystic renal mass (clear-cell renal cell carcinoma): (a) Axial post-contrast CT showing cystic masses with a smooth, minimally thickened (≤ 3 mm width) enhancing wall, with several (≥ 4) smooth thin (≤ 2 mm width) enhancing septa (arrow). (b) Axial post-contrast fat-suppressed T1WI showing an enhancing thick wall (4 mm width), with several (≥ 4) smooth thin (≤ 2 mm width) enhancing septa (arrow). The lesion was classified as category IIF by CT and category III by MRI.
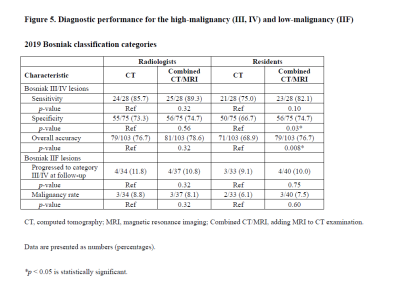
Figure 5. Diagnostic performance for the high-malignancy (III, IV) and low-malignancy (IIF) 2019 Bosniak classification categories
CT, computed tomography; MRI, magnetic resonance imaging; Combined CT/MRI, adding MRI to CT examination.
Data are presented as numbers (percentages).
*p < 0.05 is statistically significant.