3690
Predictive value of IVIM combined with DKI for breast cancer axillary lymph node metastasis: A retrospective study1the affiliated hospital of Jining medical university, Jining, China, 2GE Healthcare, MR Research China, Beijing, China
Synopsis
An accurate preoperative prediction of axillary lymph node (ALN) metastasis is essential in clinic treatment. Intravoxel incoherent motion (IVIM) and diffusion kurtosis imaging (DKI) have been reported as effective non-invasive imaging methods in reflecting internal complexity of tumors. Few studies have used DKI combined with IVIM in diagnosing ALN metastasis of breast cancer. Therefore, in this study we aimed to explore if IVIM and/or DKI was useful in evaluating the ALN metastasis.
Introduction
Axillary nodal status is an important factor of prognosis and therapeutic decision-making for patients with breast cancer[1,2]. Sentinel lymph node biopsy (SLNB) and axillary lymph nodes dissection (ALND) are currently useful methods for determining the axillary nodal status[3]. However, approximately 70% of patients without ALN metastasis were performed with ALND unnecessarily, introducing side effects of the complications affecting patients’ quality of life[4]. SLNB increases the operation time and may have false-negative results[5]. Therefore, it is necessary to find an effective non-invasive imaging method to predict ALN metastatic before surgery. DKI reflects non-Gaussian diffusive motions of water in biologic tissues. IVIM is an effective imaging technology that can obtain perfusion and diffusion parameters by using the multiple b-value , thereby better reflecting the internal situation of tumors [6,7,8]. However, no existing study has been implemented to apply combinedthe DKI and IVIM for diagnosing ALN metastasis.Therefore, this study mainly aimed to determine the clinical potential of IVIM and DKI in predicting ALN metastasis.
Materials and Methods
In total 194 patients, confirmed with breast cancer postoperatively, underwent preoperative IVIM and DKI measurement. These patients were categorized into case group (ALN metastasis) and control group (no ALN metastasis).All MR experiments were performed on a 3.0T MR scanner (Discovery MR750W, GE Medical Systems, USA) with a 16-channel phased-array breast coil. Axial fat suppression T1& T2-weighted imaging acquisitions were first performed using fast-spin-echo based sequences. Single-shot spin-echo planar-echo-imaging based was then used in DWI, IVIM and DKI. The detailed sequence parameters were listed in Table 1.
DKI and IVIM data were post-processed using vendor-provided software in GE AW4.6 workstation (GE Healthcare). DKI derived parametric maps of MD, MK and IVIM derived parametric maps of D, D*, and f were obtained accordingly. The regions of interest (ROI)s were delineated on diffusion images at b-value of 1000 s/mm2 by two radiologists, independently, and then copied on IVIM and DKI parametric maps (Fig.1). Mean value of each parameter was obtained for each ROI. In addition, conventional MRI features, including lesion morphology, T2WI signal characteristics, tumor size, lesion edge features, and enhancement methods, were also analyzed.
All statistical analyses were performed using SPSS 25.0 (IBM Corporation, Armonk, USA) and MedCalc 19.5.1 (Ostende, Belgium). Inter-observer agreement of IVIM and DKI parameter measurements between two radiologists was assessed by interclass correlation coefficients. Kolmogorov-Smirnov test was used to determine whether two groups of data have a normal distribution. Independent-sample t-test, Mann-Whitney U test, χ2 test, and Kruskal-Wallis H test were used to determine the differences of parameters between ALN and no-ALN metastasis groups. Binary Logistic regression analysis was used to determine the independent influencing factors of DKI and IVIM parameters in predicting axillary lymph node metastasis. The diagnostic efficacy of each parameter or model was evaluated by receiver operating characteristic analysis (ROC).
Results
Except for the age (the metastatic group was younger than that in the non-metastasis group (P=0.015), no other significant difference was found in the case and control groups' basic characteristics. The conventional MRI characteristics, including the tumor shape, size, margin, T2WI signal intensity, enhancement, and TIC, were compared. The edges of the lesions in the non-metastatic group tended to be clear (P=0.008).The heterogeneous enhancement and the rim enhancement accounted for a more significant proportion in the metastasis group (P=0.03). However, tumor size (P=0.007), margins (P=0.006), and enhancement (P=0.030) were significantly different. The AUC of the conventional MRI model (including the size, margin, and enhancement characteristics of lesions) for diagnosing lymph node metastasis was 0.644.The D and MD in the metastasis group were significantly lower than that of the non-metastasis group (P<0.001). The D*, f, and MK in the metastatic group were higher than that in non-metastasis group (P=0.013, 0.014, 0.001) (Fig.2). According to the binary logistic regression, D≤0.74×10-3mm2/s, D*≥39.30×10-3mm2/s, f≥35.30%, MD≤0.85×10-3mm2/s and MK≥1.30 were independent factors in predicting ALN metastasis. Among them, D value has the highest diagnostic efficacy with AUC of 0.768. Both AUC of IVIM and DKI models were higher than that of the conventional MRI model [IVIM parameters VS conventional MRI (P=0.001), DKI parameters VS conventional MRI (P=0.043)]. The accuracy and sensitivity of IVIM parameters for diagnosing lymph node metastasis were higher than that of DKI parameters (Table 2).
The AUC of IVIM combined with DKI was 0.869; this is significantly higher than IVIM (P=0.020) or DKI (P=0.001) alone. IVIM combined with DKI had an accuracy of 85.6%, a sensitivity of 81.8%, and a specificity of 89.6%, which were higher than the IVIM or DKI model (Fig. 3).
Discussion and Conclusion
In this study, we mainly investigated the predictive value of IVIM combined with DKI for breast cancer axillary lymph node metastasis. The D value in the IVIM model has the highest diagnostic efficiency. IVIM combined with DKI demonstrated higher diagnostic efficiency for ALN metastasis in breast cancer than IVIM or DKI alone.In conclusion, both IVIM model and DKI model has been demonstrated as effective tools in predicting ALN metastasis of breast cancer; this is useful for decision-making for upcoming therapies among these patients.
Acknowledgements
No acknowledgement found.References
1. Gipponi M, Bassetti C, Canavese G, et al. Sentinel lymph node as a new marker for therapeutic planning in breast cancer patients. J Surg Oncol 2004;85:102-111.
2. Peintinger F, Reitsamer R, Smidt ML, et al. Lymph Nodes in Breast Cancer-What Can We Learn from Translational Research? Breast Care (Basel) 2018;13:342-347.
3. Chang JM, Leung JWT, Moy L, et al. Axillary Nodal Evaluation in Breast Cancer: State of the Art. Radiology 2020;295:500-515.
4. Maeseele N, Faes J, Van de Putte T, et al. Axillary lymph node dissection on the run? Facts Views Vis Obgyn 2017;9:45-49.
5. Ahmed M, Purushotham AD, Douek M. Novel techniques for sentinel lymph node biopsy in breast cancer: a systematic review. Lancet Oncol 2014;15:e351-362.
6. Zhang Q, Ouyang H, Ye F, et al. Feasibility of intravoxel incoherent motion diffusion-weighted imaging in distinguishing adenocarcinoma originated from uterine corpus or cervix. Abdom Radiol (NY) 2021;46:732-744.
7. Chen W, Zhang J, Long D, et al. Optimization of intra-voxel incoherent motion measurement in diffusion-weighted imaging of breast cancer. J Appl Clin Med Phys 2017;18:191-199.
8. Iima M, Honda M, Sigmund EE, et al. Diffusion MRI of the breast: Current status and future directions. J Magn Reson Imaging 2020;52:70-90.
Figures
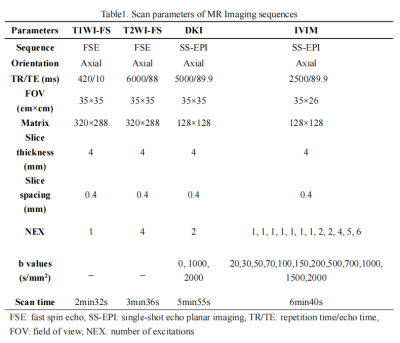
Table1. Scan parameters of MR Imaging sequences
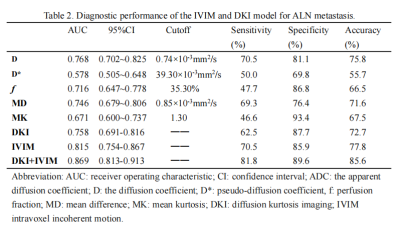
Table 2. Diagnostic performance of the IVIM and DKI model for ALN metastasis.
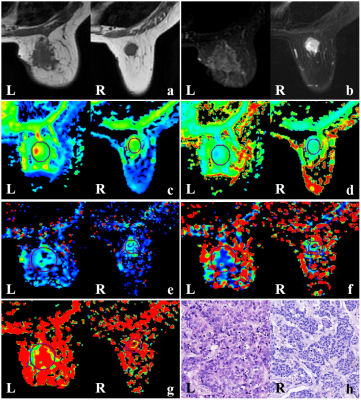
Fig.1 L: Breast cancer with axillary lymph node metastasis. a) T1WI shows low signal, b) T2WI shows uneven high signal, c) MD value is 0.27×10-3mm2/s, d) MK value is 0.702, e) D value is 0.44×10-3mm2/s, f) D* value is 44.6×10-3mm2/s, g) f value is 48.7%. h) pathological picture (HE×100). R: Breast cancer without axillary lymph node metastasis. a) T1WI shows low signal, b) T2WI shows uneven high signal, c) MD value is 0.8×10-3mm2/s, d) MK value is 1.517,e) D value is 0.62×10-3mm2/s, f) D* value is 39.5×10-3mm2/s, g) f value is 43.8%, h) pathological picture (HE×100).
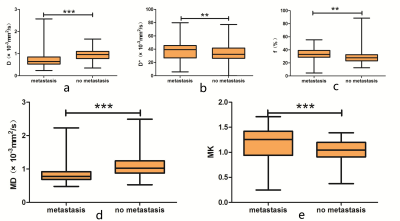
Fig.2 (a-e) Boxplots show D, D*, f, MD, and MK in breast tumors with ALN metastasis or without ALN metastasis. *P>0.05, **P<0.01, ***P<0.001.
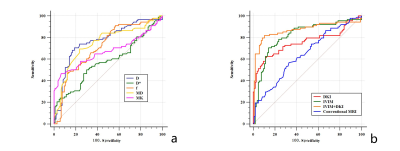
Fig.3 ROC curve analysis for MRI diagnostic efficacy. a) Comparison of diagnostic efficacy of breast cancer with lymph node metastasis, using IVIM and DKI parameters. b) Comparison of diagnostic efficacy of breast cancer with lymph node metastasis, using DKI, IVIM, DKI+IVIM and conventional MRI.