3684
The feasibility of ASL combined with Q-flow MRI in evaluating hemodynamic changes of transplant renal artery stenosis1Third Affiliated Hospital of Soochow University, Changzhou, China, 2Philips Healthcare, Shanghai, China
Synopsis
Transplant renal artery stenosis (TRAS) is a less common but important etiology of renal dysfunction following transplantation. It is of great importance to include TRAS in the differential diagnosis for allograft dysfunction early after transplantation. We used ASL combined with 2D-PC Q-flow MRI to assess hemodynamic changes of TRAS. The results reflected that there were differences in the mean flux and velocity of the stenotic segment of transplant renal artery and renal allograft perfusion between different degrees of TRAS, and the mean flux and velocity were more closely related to the degree of TRAS compared with renal allograft perfusion.
Introduction
Renal transplant artery stenosis(TRAS) is a relatively frequent complication after transplantation. Patients with a diagnosis of TRAS based on US findings underwent further MRI to refine the diagnosis with quantitative and morphological findings. The hemodynamic studies of TRAS are limited. The aim of current study is to explore the feasibility of arterial spin labeling MRI and 2D phase contrast (PC) Q-flow MRI in evaluating hemodynamic changes of TRAS.Material and Methods
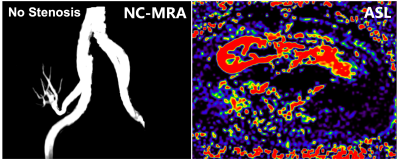
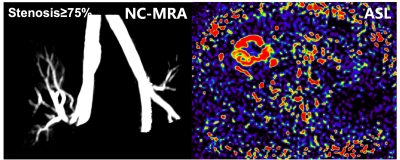
Sixty-four patients who underwent allograft renal transplantation (40 males, 24 females; age range, 20-61 years; median age, 42 years) between September 2018 and December 2020 were included in this study. All the patients underwent conventional MRI, non-contrast-enhanced magnetic resonance angiography (NC-MRA),3D pseudo-continuous arterial spin labeling(pCASL) imaging and 2D-PC Q-flow imaging were conducted on an Ingenia 3.0T MRI system(Philips Healthcare, the Netherland). The scanned objects contained renal allograft and transplant renal artery. The degree of TRAS (0, no stenosis; 1, 0<stenosis≤50%; 2, 50%<stenosis<75%; 3, stenosis≥75%) was evaluated in the NC-MRA images. The renal allograft perfusion was evaluated in the ASL images. The mean flux and velocity of the stenotic segment of transplant renal artery were calculated using the Q-flow software. Differences in renal allograft perfusion and the mean flux and velocity of the stenotic segment of transplant renal artery among the different TRAS degrees were determined using the non-parametric Kruskal-Wallis test. The relationship between the degree of TRAS with renal allograft perfusion and the mean flux and velocity of the stenotic segment of transplant renal artery was assessed by Pearson correlation coefficients.Results:
For no stenosis, the renal allograft perfusion was 223.89±64.77 ml/100g/min, the mean flux was 0.06±0.01 ml/s, and the mean velocity was 0.59±0.02 cm/s. For 0<stenosis≤50%, the renal allograft perfusion was 188.02±79.32 ml/100g/min, the mean flux was 0.11±0.23 ml/s, and the mean velocity was 3.53±0.11 cm/s. For 50%<stenosis<75%, the renal allograft perfusion was 96.45±45.05 ml/100g/min, the mean flux was 0.45±0.17 ml/s, and the mean velocity was 8.66±0.35 cm/s. For stenosis≥75%, the renal allograft perfusion was 47.40±23.98 ml/100g/min, the mean flux was 1.18±0.26 ml/s, and the mean velocity was 12.31±0.28 cm/s. The degree of TRAS was strongly correlated with the mean flux and velocity of the stenotic segment of transplant renal artery (r=0.701, P<0.001; r=0.722, P<0.001), and was moderately correlated with renal allograft perfusion (r=0.659, P=0.017).Conclusion
Arterial spin labeling MRI and 2D PC Q-flow MRI can be used to non-invasively assess hemodynamic changes of TRAS.Acknowledgements
None.References
[1] Youn SW, Kim HK, Do YR, et al. Haemodynamic alterations in cerebral blood vessels after carotid artery revascularisation: quantitative analysis using 2D phase-contrast MRI. Eur Radiol, 2013, 23(10): 2880-2890.
[2] Gondalia R, Vernuccio F, Marin D, et al. The role of MR imaging in the assessment of renal allograft vasculature. Abdom Radiol (NY), 2018, 43(10): 2589-2596.
[3] Rouer M, Godier S, Monnot A, et al. Long-term Outcomes after Transplant Renal Artery Stenosis Surgery. Ann Vasc Surg, 2019, 54: 261-268.