3680
Static-fluid MR Urography with three-dimensional Gradient and Spin-echo and Respiratory-trigger Fast Spin Echo sequences: A Comparison Study1Peking University First Hospital, Beijing, China, 2United Imaging Healthcare, Shanghai, China
Synopsis
This study is targeted to compare the performance of three-dimensional (3D) breath-hold gradient and spin-echo sequence (GRASE) and conventional respiratory-trigger fast spin-echo sequence (FSE) for magnetic resonance urography (MRU). Image quality and diagnostic performance of urinary tract dilation from two data sets were evaluated by three radiologists. The results showed that 3D GRASE MRU had a better performance compared with the FSE MRU, indicating 3D GRASE technique could be a feasible option for 3D MRU.
Introduction
The static-fluid MRU is clinically useful for quickly and directly identifying the urinary tract dilation and obstruction.1 Three-dimensional (3D) MRU could obtain contiguous thin-slice images allowing multi-plane reconstructions in any direction, and hence, providing better anatomic depiction and lesion conspicuity compared with 2D sequences. For conventional 3D respiratory-triggered fast spin-echo (RT-FSE) MRU, the most criticized point is its extra-long acquisition time. In contrast, the gradient and spin-echo (GRASE) sequence, with shorter acquisition time, could make a 3D MRU in a single breath-hold. The purpose of this study was to evaluate the performance of breath-hold GRASE (BH-GRASE) in 3D MRU.Methods
From January to May 2021, 90 patients (47 men and 43 women; mean age, 49.3±19.1 years; range, 18-87 years) were prospectively included, and underwent both 3D BH-GRASE and RT-FSE MRU at 3.0 T (uMR 790, United Imaging Healthcare, Shanghai, China). Inclusion criteria were as follows: 1) no contraindications for MRI examination, 2) completion of two types of MRU, 3) no history of urinary tract surgery, 4) visible urinary tract dilation.MR protocol for 3D BH-GRASE MRU parameters was: TR/TE=1300/ 267ms; parallel acquisition factor=3; FSE factor=35; EPI factor=7; FOV=400×400mm2; resolution (reconstruction) =1.88×1.32×3 (1.25×0.88×1.5) mm3; slice number=28; acquisition time=14.8s. For 3D RT-FSE MRU parameters: TR/TE=variable depending on respiratory/697 ms; parallel acquisition factor=2.7; FSE factor=205; FOV=400×400mm2; resolution (reconstruction) =1.42×1.14×2 (0.95×0.76×1) mm3; slice number=42; acquisition time=variable (range: 132–392s).
Three readers blinded to the MR protocols reviewed the source and MIP images. Reader A and B qualitatively evaluated the image quality using a five-point scale, including the overall image quality, artifact, urinary tract visualization. Reader B and C assessed the diagnostic performance related to urinary tract dilation, based on the degree of dilation, obstructive location, and imaging features (benign or malignant) at the obstructive site. The relative contrast ratio (CR) between the urinary tract and adjacent area was measured quantitatively by Reader C.
CR=(SIU-SIA) / (SIU +SIA)
where SIU and SIA stand for the signal intensities of the urinary tract and adjacent area, respectively. The acquisition time of two MRU protocols was recorded by Reader C. The reference standard was confirmed by the clinical data and the pathological results of the endoscope biopsy or surgery.
Results
The reference standard for the diagnosis of urinary tract pathology was based on subsequent surgery (n=22), endoscope (n=22). Of these, 21 were diagnosed with malignant lesion and 23 had benign stricture. The remaining 46 patients were clinically diagnosed due to benign consideration based on clinical information.Overall, no significant difference were found for image quality between two MRU protocols. 3D BH-GRASE MRU better depicted bilateral renal calyces than RT-FSE MRU (p<0.05), Table 1.
For the quantitative evaluation of urinary tract contrast, CR values were slightly lower on BH-GRASE MRU (CRpelvis=0.81±0.13; CRureter=0.91±0.12; CRbladder=0.93±0.03) compared with RT-FSE MRU (CRpelvis=0.86±0.09; CRureter=0.95±0.04; CRbladder=0.96±0.02; all p values<0.05).
There were excellent agreements in the assessment of urinary tract dilation between two MRU protocols, including the dilated degree, the obstructive level, and the obstructive imaging features (inter-sequence κ=0.924-1). 3D BH-GRASE MRU achieved comparable diagnostic ability for diagnosing the etiology of obstruction with RT-FSE MRU (Fig. 1,2, Table 2).
Discussion
In this study, the performance of two different MRU methods, based on BH GRASE and RT-FSE respectively, was compared qualitatively and quantitatively. 3D MRU was successfully performed within a single breath-hold using the GRASE technique.The GRASE sequence, proposed in the early 1990s, is a combination of spin- and gradient-echo sequence.2 It provides shorter acquisition time than conventional FSE, due to the interleaving of the EPI readout between two consecutive 180 pulse (Fig. 3). In this study, 3D MRU was accelerated by adopting a FSE factor of 35, an EPI factor of 7, and a SENSE factor of 3. Acceleration of 3D MRU not only increases patient tolerance, but also decreases the motion-related artifacts of renal calyces.
As the multi-parametric MR urography requires a coverage of the entire urinary tract from abdomen to pelvic with several types of sequences,3 it is usually time-consuming, about 30 to 40min. As the 3D BH-GRASE MRU is quick and easy to perform, adding it into the routine multi-parametric MR urography protocol may provide not only a broad overview of the urinary tract, but also more diagnostic information.
Conclusion
Our study demonstrates the clinical feasibility of BH-GRASE in 3D static-fluid MRU for depicting the urinary tract obstruction and dilation, as it could be performed in a single a breath-hold without sacrificing image quality and diagnostic performance. BH-GRASE sequence could be a preferred clinically feasible protocol for 3D MRU.Acknowledgements
We thank Yanqun Teng and Shuheng Zhang of United Imaging Healthcare for the technical support.References
1. Kadam D, Patil S, Dhok A, Jain M (2019) MR urography in evaluating obstructive uropathy: one stop shop. Int Surg J 6:944. https://doi.org/10.18203/2349-2902.isj20190829
2. Feinberg DA, Oshio K (1991) GRASE (Gradient- and Spin-Echo) MR imaging: A new fast clinical imaging technique. Radiology 181:597–602. https://doi.org/10.1148/radiology.181.2.1924811
3. Rouvière O, Cornelis F, Brunelle S, et al (2020) Imaging protocols for renal multiparametric MRI and MR urography: results of a consensus conference from the French Society of Genitourinary Imaging. Eur Radiol 30:2103–2114. https://doi.org/10.1007/s00330-019-06530-z
Figures
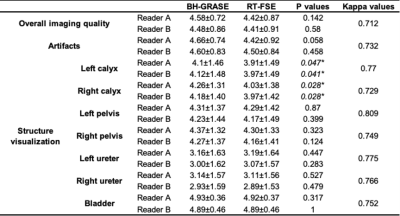
Table 1 Qualitative analysis scores of the two MRU protocols. *P value with significance. BH-GRASE: breath-hold gradient and spin-echo; RT-FSE: respiratory-triggered fast spin-echo
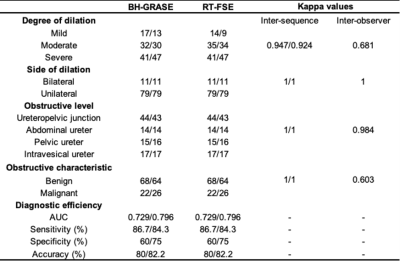
Table 2 Diagnostic performance of the two MRU protocols (Reader B/Reader C). BH-GRASE: breath-hold gradient and spin-echo; RT-FSE: respiratory-triggered fast spin-echo; AUC: area under the curve

Figure 1 A 49-year-old male with right UPJO. The visualization of dilated right renal calyces and pelvis are blurred due to motion artifact in RT-FSE MRU (a, c,), whereas 3D BH-GRASE MRU (b, d,) display them clearly(arrows). The acquisition times were 5 min 8 s for 3D RT-FSE MRU and 14.8s for the 3D BH-GRASE.
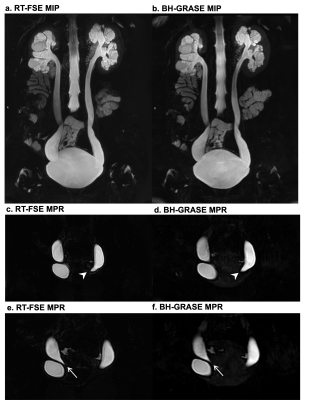
Figure 2 A 27-year-old female with bilateral ureterovesical junction obstruction. The coronal MIP and MPR images of RT-FSE (a,c,e) and BH-GRASE MRU (b,d,f) allow good visualization of diffuse dilation of upper urinary tract and clearly displayed the beak-like stenosis of both ureters.
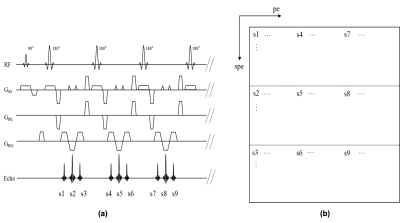
Figure 3 The 3D GRASE pulse sequence with EPI factor = 3. Each refocusing pulse can acquire three echoes (a). In the k-space, echoes are filled sequentially in spe direction(b). In addition, s1, s4, and s7 belong to different TSE factor and filled in different part in pe direction.