3675
Diagnostic performance of transition zone prostate cancer: a comparison between PI-RADS v2.1 and PI-RADS v21The Department of Radiology, The General Hospital of Ningxia Medical University, Yinchuan, China, 2GE Healthcare,MR Research, Beijing, China
Synopsis
In this study, we aim to investigate the diagnostic value of PI-RADS v2.1 and PI-RADS v2 (prostate imaging reporting and data system version 2.1 and version 2) in diagnosing transition zone prostate cancer. It was concluded that the diagnostic value of PI-RADS v2.1was not lower than that of PI-RADS v2.
Introduction
Prostate cancer is the first malignant tumor for men in the United States[1], and the incidence of prostate cancer in China has increased remarkably in recent years[2]. At present, multi-parametric magnetic resonance imaging (mp-MRI) is the most common imaging method for the diagnosis and risk stratification of prostate cancer[3-4]. In order to simplify and standardize the professional terms in radiological reports, prostate imaging reporting and data system version 2 (PI-RADS v2) was released in 2015[5]. However, limitations such as poor consistency among physicians and ambiguity in scoring criteria have been recognized[6-7] triggered an upgraded version,PI-RADS v2.1 in 2019[8]. However, at present, there are few studies on the diagnostic performance of PI-RADSv2.1 in transition zone prostate cancer domestic and abroad. Therefore, the purpose of this study was to explore diagnostic performance of PI-RADS v2.1 and PI-RADS v2 for transition zone Prostate cancer(PCa)and clinically significant prostate cancer(csPCa).Material and Methods
From Jan 2017 to Jun 2020, the clinical and imaging data of 108 patients with lesions located in the transitional zone(53 cases of prostate cancer, 55 cases of benign prostatic hyperplasia and / or inflammation) confirmed by pathology were analyzed retrospectively in our study. Prostate cancer group: age range 54-82 years old, median age 70 years old, prostate specific antigen (PSA) 0.169-100μg/L, median PSA 47.26μg/L. Benign hyperplasia and / or inflammation group(Benign prostatic lesions group): age range 49-81 years old,median age 66 years old, PSA range 0.396-29.46 μg/L, median PSA 14.20 μg/L. All patients underwent MRI examination on a 3.0T scanner (Philips 3.0T Ingenia MR, Holland) and 32-channel body phase coil before puncture biopsy or radical operation. The scan sequences included axial T1-weighted、T2-weighted、T2 flair-weighted,sagittal T2-weighted 、coronal T2-weighted imaging ,axial Diffusion-weighted imaging and axial Dynamic contrast enhanced(DCE)imaging. Two radiologists were trained by PI-RADS v2.1 and PI-RADS v2 (radiologist 1 and radiologist 2, with 8 and 3 years' experience in prostate diagnosis respectively), who were blinded to the pathological results and PSA levels, independently used PI-RADS v2.1 and PI-RADS v2 to score the transitional zone lesions. The interval between the first and second scoring by the readers is not less than 4 weeks. Kappa test was used to assess the consistency of the scoring results between two radiologists. ROC curve was used to evaluate and calculate the diagnostic efficiency for transition zone PCa and csPCa. Spearman correlation analysis was used to analyze the correlation between the scoring results and Gleason score. csPCa was defined as puncture or pathological gross Gleason score ≥ 7 (including 3+4); and / or lesion volume ≥ 0.5cm ³; and / or extracapsular invasion of the prostate.Results
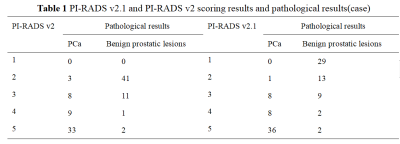
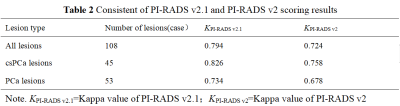
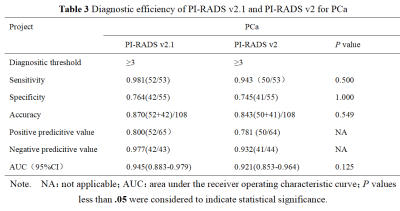
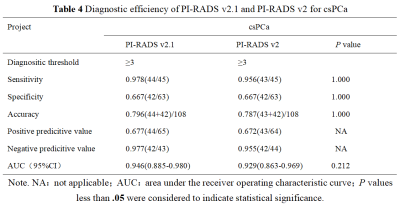
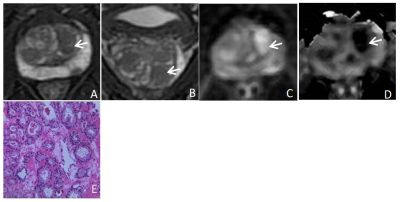
There were 55 cases of benign prostatic hyperplasia and / or inflammation, and 53 cases of PCa, of which 45 cases were csPCa(Table 1). The consistency of PI-RADS v2.1 was improved compared with PI-RADS v2 (Table 2). The sensitivity, accuracy and AUC of PI-RADS v2.1 in diagnosing PCa and csPCa and specificity of PI-RADS v2.1 in diagnosing PCa were slightly higher than those of PI-RADS v2 , but the difference was not significant(all P> 0.05); Positive predictive value and negative predictive value of PI-RADS v2.1 in diagnosing PCa and csPCa were slightly higher than those of PI-RADS v2(Table 3、4,Figure 1). The scoring results of PI-RADS v2.1 and PI-RADS v2 were moderately positively correlated with Gleason score (r=0.552 vs. r=0.507,P <0.05)PI-RADS v2 missed 2 cases csPCa,while PI-RADS v2.1 missed 1.Discussion and Conclusion
Radiologists,consistency of PI-RADS v2.1 was better, in agreement of previous study by Tamada et al [9]. The diagnostic efficiency of PI-RADS v2.1 for PCa and csPCa was slightly higher than PI-RADSv2, but the difference was not statistically significant. The result of Yang Shuo et al [10] showed that AUC value of PI-RADS v2.1 in diagnosing PCa and csPCa were slightly higher than PI-RADS v2, though not statistically significant, which was consistent with the results of this study. When using the PI-RADS 3 score as the puncture indication, PI-RADS v2 missed 2 cases csPCa,while PI-RADS v2.1 missed 1, which may be related to the upgrading of some atypical nodules from 2 score to 3 score. The scoring results of PI-RADS v2.1 and PI-RADS v2 were both moderately positively correlated with Gleason score, indicating that PI-RADS system is helpful to predict the biological behavior of prostate cancer. One of the major limitations in our study is that the number of samples is too small. Therefore, a large sample study is needed in the future. To conclude, PI-RADS v2.1 has better consistency, diagnostic efficiency is not lower than PI-RADS v2, and helps to reduce the missed diagnosis of csPCa; PI-RADS system helps to evaluate the invasiveness of tumors, which is conducive to clinical diagnosis and treatment decisions.Acknowledgements
We thank wiley for all physicians,assistance of The Department of Radiology, The General Hospital of Ningxia Medical University during the preparation of this manuscript. We thank all of the participants of this study. We also acknowledge the support provided by Dr.Xiaocheng Wei from GE Healthcare. Beijing,China.References
1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020,70(1):7-30.
2.Feng RM,Zong YN,Cao SM,et al. Current cancer situation in China: good or bad news from the 2018 Global Cancer Statistics?[J]. Cancer Communications,2019,39(1).
3.Wang YR, Guo QY, Yu B, et al. Current status and prospect of multi-parameter magnetic resonance imaging in the evaluation of prostate cancer [J]. Practice of Radiology, 2018,33 (12): 1339-1342.
4.Stabile A,Giganti F,Rosenkrantz AB ,et al. Multiparametric MRI for prostate cancer diagnosis: current status and future directions.[J] .Nat Rev Urol, 2020, 17(1): 41-61.
5.Weinreb JC, Barentsz JO, Choyke PL, et al. PI-RADS prostate imaging-reporting and data system: 2015, version 2. Eur Urol,2016, 69(1): 16-40.
6.Gupta RT,Mehta KA,Turkbey B,et al. PI-RADS: Past, present, and future.[J] .J Magn Reson Imaging, 2020, 52(1): 33-53.
7.Smith CP, Türkbey B. PI-RADS v2: Current standing and future outlook.Turk J Urol 2018,44(3):189-194.
8.Turkbey B, Rosenkrantz AB, Haider MA, et al. Prostate imaging reporting and data system version 2.1: 2019 update of prostate imag-ing reporting and data system version 2. Eur Urol 2019,76(3):340-351.
9.Tamada T,Kido A,Takeuchi M,et al. Comparison of PI-RADS version 2 and PI-RADS version 2.1 for the detection of transition zone prostate cancer.[J] .Eur J Radiol, 2019, 121: 108704.
10.Yang S, Zhang CY, Zhang YY, et al.The diagnostic value of version 2.1 prostate imaging reporting and data system for prostate transitional zone lesions[J].Chinese Medical Journal,2020,100(45):3609-3613.
Figures