3670
A preliminary study of optimized b-value scheme in diagnosis of cervical cancer using reduced field-of-view diffusion weighted imaging1Biomedical Engineering College, Hubei University of Medicine, Hubei, China, 2GE Healthcare, Beijing, China, 3Department of Radiology,Taihe Hospital, Hubei University of Medicine, Hubei, China
Synopsis
The number of used b values and the b values themselves prolong scan time. Longer scan time deprives patient tolerance, increase more possibility of involuntary movement, and thus limits the application value of IVIM technology. Therefore, we aimed to explore the optimal scheme of rFOV DW imaging with multiple b-values. We found no significant difference of mean ADC, D* and f values but mean D value in our patients between two different b-value schemes, suggesting optimized b-value setting was appropriate in diagnosis of cervical cancer especially for cervical squamous carcinoma.
Introduction
Cervical cancer is a common malignant tumor in female reproductive system. Incidence and mortality of female cervical cancer respectively reaches up to 6.5% and 7.7% in 2020[1]. IVIM-derived parameters, including diffusion coefficient (D), pseudo diffusion coefficient (D*) and perfusion fraction (f), are of great significance for the detection and diagnosis of cervical cancer. In terms of cervical cancer, there is no clear evidence of ideal b-value selection, usually 10-13 b-values, to compute parameters for better diagnosis and prognosis [2]. Noteworthily, the number of used b values and the b values themselves prolong scan time. Longer scan time deprives patient tolerance, increase more possibility of involuntary movement, and thus limits the application value of IVIM technology. Reduced field-of-view (rFOV) DWI offers less image distortion and artifact so as to improve diagnosis and treatment of cervical cancer [3], but there is no literature of rFOV DWI with optimized b-value selection to provide accurate clinical diagnosis and treatment plans with advantage of short scan time. Therefore, in this study, we aimed to explore the optimal scheme of rFOV DW imaging with multiple b-values for the cervical cancer without affecting image quality and diagnostic accuracy and with advantage of higher space resolution and shorter scan time.Materials and methods
25 cervical cancer patients were recruited in our study after signing written informed consent. All patients underwent axial diffusion weighted imaging with two b schemes (TR/TE =4000/71.6ms, FOV = 22 cm, slice thickness = 4 mm, 5 b-values: 0,100,400,800,1500, scan time about 4 min ;13 b-values: 0-100,150,200-1200, 1500,scan time about 11 min) on 1.5T MR scanner (Signa Voyager, GE Healthcare) after properly emptying the bladder to reduce intestinal peristalsis artifacts and urine electrolyte artifacts. All data were post-processed on GE 4.6 Workstation. All parameter maps, including standard ADC, pure diffusion coefficient (D), pseudo diffusion coefficient (D*), perfusion fraction (f) were computed for ROI drawing on the largest cross-section by one experienced radiologist who was double-blinded to patient information. All values were compared using paired T test or Wilcoxon signed rank test depending on data normality by Shapiro-Wilk test. P<0.05 was considered statistically significant. The receiver operating characteristic (ROC) curves of each quantitative parameters in differentiation of two groups were computed at maximal Youden index for sensitivity, specificity, and area under the curves for diagnosis efficiency.Results
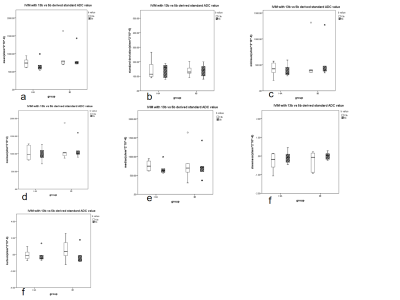
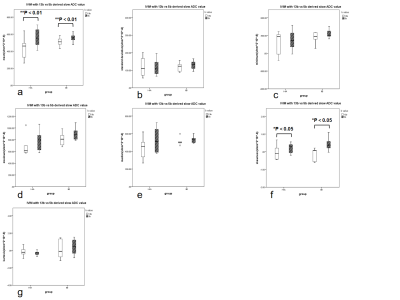
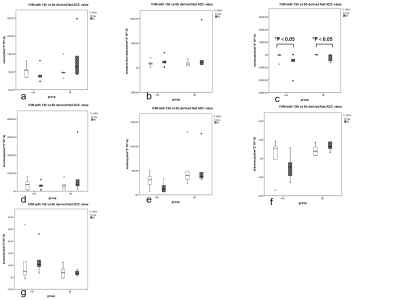
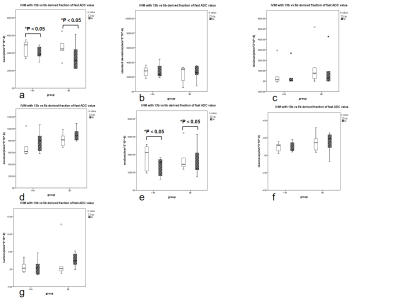
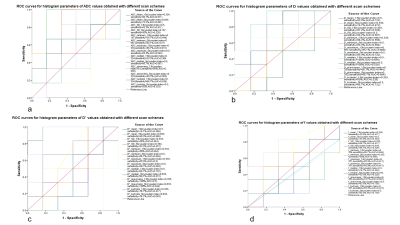
There was no significant difference of histogram-analyzed parameters between ADC maps computed by IVIM with two different b-value schemes (p > 0.05) (Figure 1). There were significant different mean and skewness between D map, minimum between D* map, median and minimum between f map computed by IVIM with two different b-value schemes (p < 0.05) (Figure 2, 3, 4). AUC of 13b and 5b showed ADC and D had the highest diagnostic efficiency (Figure 5). IVIM with 5 b-value scheme generates many histogram-analyzed parameters with better differentiation performance than IVIM with 13 b-value scheme, including mean, median, maximum, minimum, skewness of ADC map, median, skewness, kurtosis of D map, mean, SD, maximum, median, skewness of D* map, and SD, median, skewness, kurtosis of f map.Discussion
We found no significant difference of mean ADC, D* and f values but mean D value in our patients between two different b-value schemes, suggesting optimized b-value setting was appropriate in diagnosis of cervical cancer especially for cervical squamous carcinoma. Le Bihan et al [4] have shown that at least four different b values (including b=0 s/mm²) must be used to extract IVIM related parameters (D, D*, f). Andreas Lemke et al [5] described the optimal b-value selection is necessary for abdominal organs. The reason for stable images and better reproducibility of the optimized b-value scheme might attribute to the fewer number of b-values, shortened scanning time, increased patient tolerance, and reduced probability of involuntary motion. Another reason for the better results of the simplified b-value scheme in the application of cervical cancer is the combination of rFOV-DWI imaging [6] and optimized b-value used for IVIM, which eliminated the disadvantage that conventional diffusion imaging is susceptible to respiratory motion, involuntary motion artifact of intestine and chemical shift artifact. In this optimized IVIM protocol, it improved the reproducibility of the simplified b-value model with the unique advantages of reduced FOV while maintaining an original large acquisition matrix, improved resolution and decreased magnetic sensitive artifacts and motion artifacts [7]. A limitation but also positive effect on this study is that small sample size and patients with similarly altered tissue structure such as cervical squamous carcinoma were used, leading to excellent intra-modality consistency of parametric values but poor diagnostic performance as IVIM with 13b-value scheme.Conclusions
The optimal b value scheme for IVIM in our study had a potential to sustain diagnosis efficiency in cervical squamous carcinoma and also benefit to patients with shorter scan time and comfort.Acknowledgements
No acknowledgement found.References
[1]. Hyuna, S., et al., Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians, 2021. 71(3).
[2]. Chen, W., et al., Optimization of intra-voxel incoherent motion measurement in diffusion-weighted imaging of breast cancer. Journal of Applied Clinical Medical Physics, 2017. 18(3): p. 191-199.
[3]. Chen, M., et al., Comparison of reduced field-of-view diffusion-weighted imaging (DWI) and conventional DWI techniques in the assessment of Cervical carcinoma at 3.0T: Image quality and FIGO staging. European Journal of Radiology, 2021. 137(Jun (6)): p. 109557.
[4]. Bihan, D.L., et al., Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology, 2006.: p. 497-505.
[5]. Lemke, A., et al., Toward an optimal distribution of b values for intravoxel incoherent motion imaging. Magnetic Resonance Imaging, 2011. 29(6): p. 766-776.
[6]. Dong,H.B.,et al.,Application of Reduced Field-of-View Diffusion Weighted Imaging in the Diagnosis of Breast Cancer.Journal of Clinical Radiology,2015:p.360-363.
[7].Deng ,B.D.,et al.,Clinical value of reduced field-of-view diffusion-weighted imaging in cervical cancer.Chinese Journal of Magnetic Resonance Imaging,2020:p.487-492
Figures