3668
Cervical carcinoma: Evaluation using diffusion MRI with a fractional order calculus model and its correlation with histopathologic findings1Department of Radiology, Fourth Hospital of Hebei Medical University, Shijiazhuang, China, 2United Imaging Healthcare, Shanghai, China, 3Shanghai Key Laboratory of Magnetic Resonance, Department of Physics, East China Normal University, Shanghai, China
Synopsis
Clear insights into histological subtype and differentiation grade are essential in cervical carcinoma diagnosis and management. In current study, we demonstrated the feasibility of using high-b-value non-Gaussian diffusion model fractional order calculus (FROC) model to differentiate the tumor subtype and grade of cervical carcinoma. FROC model provided a set of novel diffusion parameters and the combination of these parameters contributed to the best diagnostic performance in differentiation between low-grade and high-grade cervical carcinoma.
Introduction
The two main histological subtypes, squamous cell carcinoma (SCC) and adenocarcinoma (ACA), account for approximately 70% and 25% of all cervical cancers, respectively [1]. According to previous studies, the different cell types probably have different patterns of failure and survival [2]. The aggressiveness of tumors represented by histological differentiation grade can also provide critical information for selecting treatment plans. Therefore, the clear insights into histological subtype and differentiation grade are essential in cervical carcinoma diagnosis and management. Previous studies have reported the potential use of apparent diffusion coefficient (ADC) derived from diffusion-weighted imaging (DWI) to evaluate cervical carcinoma subtype and grade [3, 4]. However, this conventional mono-exponential MRI method lacks specific parameters mirrors tumor microstructures, which are essential for assessing tumor subtype and grade. In this study, we aimed to investigate the feasibility of using fractional order calculus (FROC) model to reflect tumor subtype and grade of cervical carcinoma.Methods
Study populationSixty patients (age, 53.0 ± 10.1) were enrolled. All cases involved in this study were confirmed to have cervical carcinoma by biopsy. Histological subtype was separated into SCC and ACA. Besides, all the cases were classified into a high-grade tumor group (poorly differentiated tumor) and a low-grade tumor group (well- or moderately differentiated tumor).
MR Imaging
All the MRI examinations have been overtaken on a 3.0T MR scanner (uMR 780, United Imaging Healthcare, Shanghai, China) with a commercial 12-channel body phased array coil. MR sequences included: 1) axial T1-weighted (T1W) fast spin echo (FSE) sequence; 2) axial T2-weighted (T2W) FSE sequence; 3) coronal fat-suppressed T2W FSE sequence; 4) sagittal T2W FSE sequence; and 5) diffusion weighted imaging with a series of b-value 0, 20, 40, 80, 160, 200, 500, 1000, 2000 s/mm2.
Image analysis
The conventional mono-exponential model was applied to compute ADC by using images from two b-values, 0 and 1000 s/mm2. The voxel intensity is given by
$$$S=S0exp[-bADC]$$$ (1)
where S0 is the signal intensity without diffusion weighting and b is the diffusion-sensitizing factor.
The FROC model was set up following the equation (2) [5]
$$$S=S0exp[-Dμ2(β-1)(γGdδ)2β(Δ-(2β-1)/(2β+1)δ)]$$$ (2)
where Gd is the diffusion gradient amplitude. The FROC model in Eq. (2) contains three parameters: an anomalous diffusion coefficient D, an intravoxel diffusion heterogeneity parameter β, and a spatial parameter μ.
The volumes of interest (VOIs) were placed on the solid regions of tumors to avoid confounding effects caused by other tissue compositions, such as necrosis and calcification. The VOIs were first determined on the diffusion-weighted images with b = 0, and then propagated to the corresponding D, β, μ, and ADC map. The mean values of D, β, μ, and ADC were recorded.
Statistics
The subtype differences and differentiation grade differences were evaluated by Mann-Whitney U test. Receiver operating characteristic (ROC) analyses were performed to assess the diagnostic performance and determine the best predictor for both univariate analysis and multivariate analysis. P-value < 0.05 was considered as indicating statistically significant difference. Bonferroni corrections were applied to reduce problems associated with multiple comparisons.
Results
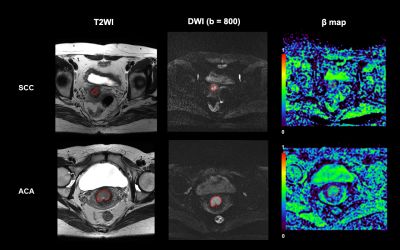
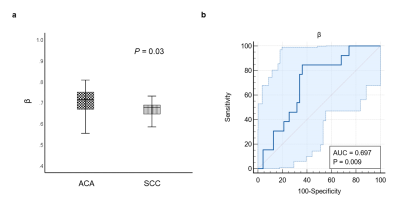
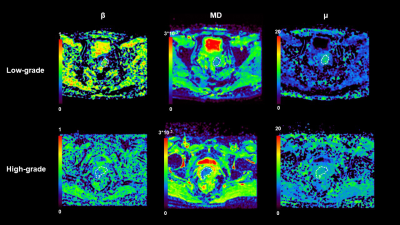
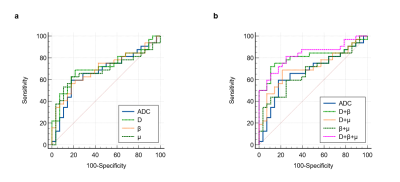
Figure 1 shows a set of representative images from patients with SCC and ACA, respectively. Only the β derived from FROC model could differentiate different cervical carcinoma subtype (P = 0.03 < 0.05) and the squamous cell carcinoma (SCC) lesion exhibited significant lower β value than the adenocarcinoma lesion (Figure 2). Figure 3 shows a set of representative images from patients with low-grade and high-grade cervical carcinoma, respectively. As shown in Figure 4, all the individual parameters, including mean ADC as well as β, D and μ derived from FROC model, could differentiate low-grade cervical carcinoma from high-grade cervical carcinoma (P = 0.022, 0.009, 0.004 and 0.015, respectively). As shown in Figure 5b, the combination of all the FROC parameters showed the best overall performance, providing the highest sensitivity (81.2%) and AUC (0.829). Besides, the combination of D and β showed the highest specificity (89.3%) and accuracy (80.0%).Discussion & Conclusion
Our result reflected a significant increase in microscopic tissue heterogeneity from SCC to ADC, which was inline with previous diffusion kurtosis imaging (DKI) research and conventional DWI studies in cervical carcinoma [6]. Besides, in present study, the high-grade lesion exhibited significant lower mean ADC, β, D and μ value than the low-grade lesion and the mean value of D derived from FROC model provided the best individual parameter performance in grading the tumors when compared with the other diffusion parameters. Prior conventional DWI studies supported our findings that mean value of ADC was negatively correlated with tumor grades of cervical carcinoma [7, 8]. These results could be explained by the aggressiveness of cervical carcinoma. The combination of all the FROC parameters showed the best overall performance in grading the cervical carcinoma, producing the highest sensitivity and AUC. The D+β showed the highest specificity and accuracy. These multivariate analysis results further suggested that a noninvasive DWI-based classifier that reflects tumor grade of cervical carcinoma can be developed.Acknowledgements
No acknowledgement found.References
1. De Juan, A., et al., SEOM clinical guidelines for cervical cancer (2019). Clinical and Translational Oncology, 2020. 22(2): p. 270-278.
2. Hong, J., et al., Comparison of clinical behaviors and responses to radiation between squamous cell carcinomas and adenocarcinomas/adenosquamous carcinomas of the cervix. Chang Gung medical journal, 2000. 23(7): p. 396-404.
3. Exner, M., et al., Value of diffusion-weighted MRI in diagnosis of uterine cervical cancer: a prospective study evaluating the benefits of DWI compared to conventional MR sequences in a 3T environment. Acta radiologica, 2016. 57(7): p. 869-877.
4. Kuang, F., et al., The value of apparent diffusion coefficient in the assessment of cervical cancer. European radiology, 2013. 23(4): p. 1050-1058.
5. Zhou, X.J., et al., Studies of anomalous diffusion in the human brain using fractional order calculus. Magnetic resonance in medicine, 2010. 63(3): p. 562-569.
6. Wang, M., et al., Diffusion kurtosis imaging in the assessment of cervical carcinoma. Academic radiology, 2020. 27(5): p. e94-e101.
7. Liu, Y., et al., Diffusion-weighted magnetic resonance imaging of uterine cervical cancer. Journal of computer assisted tomography, 2009. 33(6): p. 858-862.
8. Liu, Y., et al., Clinical application of diffusion-weighted magnetic resonance imaging in uterine cervical cancer. International Journal of Gynecologic Cancer, 2015. 25(6).
Figures