3661
O2-inhalation T2* BOLD and dual-VENC 4D flow MRI: hypoxic evaluation of pediatric transplanted kidneys1Tokyo Women's Medical University, Tokyo, Japan, 2Philips Japan, Tokyo, Japan
Synopsis
For pediatric patients with end-stage renal failure, kidney transplantation is the only treatment that can provide growth and long-term survival. Although rejection is the common cause of renal dysfunction, there are other causes of chronic transplant nephropathy, in which the transplanted kidney develops fibrosis. Hypoxia is considered as possible causes of this order. We used O2-inhalation T2*-BOLD and dual-VENC 4D flow MRI to assess hypoxia in pediatric transplanted kidneys. In patients with chronic transplant nephropathy, hypoxia was found in the renal medulla and small vessel’s flow was reduced. This analysis is an effective means of monitoring hypoxia in transplanted kidneys.
Objectives
Tissue hypoxia plays a key role in the development of progressive dysfunction and fibrosis in transplanted kidneys. Blood-oxygen-level-dependent (BOLD) MRI is the most promising imaging technique to monitor tissue oxygenation in vivo. 4D flow MRI allows non-invasive evaluation of blood flow in the transplanted kidney without contrast medium. We used a hybrid of these two approaches to assess tissue oxygenation in pediatric transplanted kidneys and compared it between the presence and absence of chronic transplant nephropathy evidenced by renal biopsy.Methods
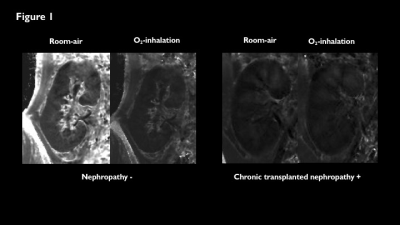
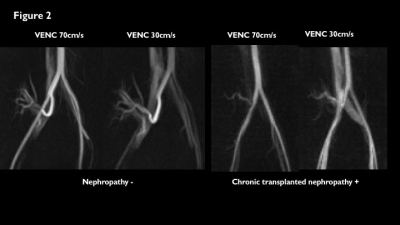
Data of O2-inhalation T2*-BOLD and dual-velocity encoding (VENC) 4D flow MRI for transplanted kidney collected from 4 patients (mean age, 12 years) using a 3-tesla scanner (Ingenia 3T CX, Philips Healthcare) were prospectively analyzed. T2*-BOLD was conducted using the black blood, breath-hold, and multi-echo gradient-echo sequence. Over 10 min inhalation of oxygen at the flow rate of 10 L/min, R2* for a region of interest in the renal cortex and medulla was measured following room-air and oxygen inhalation (Fig. 1). ΔR2*(ms-1) and ΔR2*ratio (R2*oxy-R2*air / R2*air, %)were calculated, and defined as estimates of renal oxygenation (Ref. 1). A free-breathing 4D flow sequence with echo-planar imaging was used as 4D flow (Ref. 2 and 3). The VENC was set to 30 cm/s and 70 cm/s, and rotational reconstructed images of the transplanted renal vessels were created immediately after the acquisition (Fig. 2) (Ref. 4).Results & Discussion
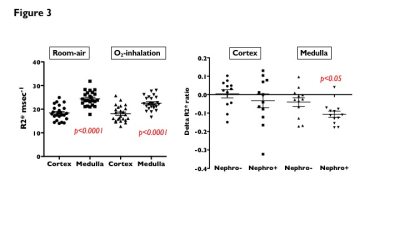
Renal biopsies showed chronic transplant nephropathy with fibrosis in two of the four patients. In all patients, R2* was significantly lower for renal cortex than that for renal medulla both under room-air and after oxygen inhalation (room-air, 18.4±3.1ms vs. 24.4±3.1ms; O2-inhalation, 18.1±3.3ms vs. 22.5±2.9ms; p<0.0001) (Fig. 3). ΔR2*ratio in renal medulla was significantly lower for patients with chronic transplant nephropathythan those without (-10.7±5.9 % vs. -4.0±8.1 %; p<0.05).ΔR2*ratio in renal cortex was lower for patients with chronic transplant nephropathythan those without (-3.3±12.9 % vs. 0.4±7.7 %), but there was no significant difference (Fig. 3). In the 4D flow with VENC 70 cm/s, the flow of the transplanted renal artery was delineated in all four patients. 4D flow with VENC 30 cm/s showed clearly small arteriovenous flow in the transplanted kidney in patients without chronic transplant nephropathy, while the small vessels’ flow in the renal parenchyma reduced in a patient with chronic transplant nephropathy (Fig. 2).In chronic transplant nephropathy, inhalation of oxygen does not cause oxygen-induced vasoconstriction because the vascular endothelium is damaged. This results in an increase in stagnant oxy-hemoglobin in the microvascular beds of the renal parenchyma. An increase in oxy-hemoglobin, i.e., a decrease in R2*, is considered a finding indicating impaired tissue oxygenation (Ref. 1). Although renal arterial flow was maintained on 4D flow with a VENC 70 cm/s, small vessels’ flow disappeared in the central part of the transplanted kidney on VENC 30 cm/s. This is consistent with a pronounced tendency for hypoxia in the renal medulla from O2-inhalation T2*-BOLD analysis.Conclusion
In patients with chronic transplant nephropathy, hypoxia was found in the main body of the renal medulla, and small vessel’s flow in the renal parenchyma was reduced. This hybrid MRI analysis is an effective means of monitoring hypoxia and ischemia in transplanted kidneys before they progress to fibrosis, and is a non-invasive alternative to kidney biopsy.Acknowledgements
This work was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI (19K08209).References
1. Ando K, Nagao M, Watanabe E, et al. Association between myocardial hypoxia and fibrosis in hypertrophic cardiomyopathy: analysis by T2* BOLD and T1 mapping MRI. Eur Radiol 2020; 30: 4327-36.
2. Tsuchiya N, Nagao M, Shiina Y, et al. Circulation derived from 4D flow MRI correlates with right ventricular dysfunction in patients with tetralogy of Fallot. Sci Rep 2021 DOI:10.1038/s41598-021-91125-2.
3. Shiina Y, Inai K, Nagao M. Non-physiological aortic flow and aortopathy in adult patients with transposition of the great arteries after the Jatene procedure: a pilot study using echo planar 4D flow MRI. Magn Reson Med Sci 2021 DOI: 10.2463/mrms.mp.2020-0101
4. Shiina Y, Kawakubo M, Inai K, Nagao M. Dual VENC 4D flow magnetic resonance imaging demonstrates arterial-pulmonary collaterals in an adult with tetralogy of Fallot. Eur Heart J Cardiovasc Imaging 2020 DOI: 10.1093/ehjci/jeaa343.
Figures