3612
Altered resting-state cerebral blood flow and functional connectivity mediate suicidal ideation in major depressive disorder1Department of Neurology, Affiliated ZhongDa Hospital, School of Medicine, Southeast University, Nanjing, China, 2Neuropsychiatric Institute, Affiliated ZhongDa Hospital, Southeast University, Nanjing, China, 3The Key Laboratory of Developmental Genes and Human Disease, Southeast University, Nanjing, China
Synopsis
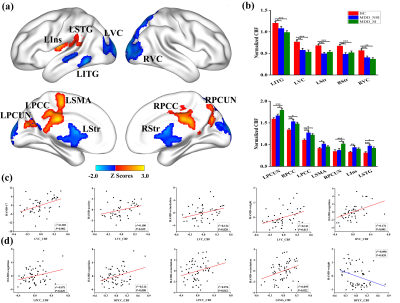
The relationship among cerebral blood flow (CBF), functional connectivity (FC), and suicidal ideation (SI) in MDD patients has been elusive. 175 participants including 47 MDD without SI (MDDNSI), 59 MDD with SI (MDDSI), and 69 controls (HC) underwent ASL, resting-state fMRI scans, and completed neuropsychological tests. Results showed that CBF was increased in MDDSI patients in the bilateral precuneus. MDDSI patients exhibited enhanced FC in the prefrontal-limbic system and decreased FC in the right precentral gyrus relative to MDDNSI patients. Mediation analyses identified that the FC could mediate the association between CBF and behavioral performance in subgroups.
METHODS: Total 175 participants including 47 MDD without SI (MDDNSI), 59 MDD with SI (MDDSI), and 69 healthy control (HC) subjects underwent arterial spin labeling MRI and resting-state functional MRI scans, and completed neuropsychological tests. Then, the whole-brain voxel-wised CBF and seed-based FC were measured. Partial correlation analyses were used to determine the correlations of the regional CBF and FC alterations with behavioral performance. Mediation analysis was further employed to identify the potential effects of FC on the association between abnormal CBF in the specific regions and behavioral performance in MDD subgroup patients, respectively.
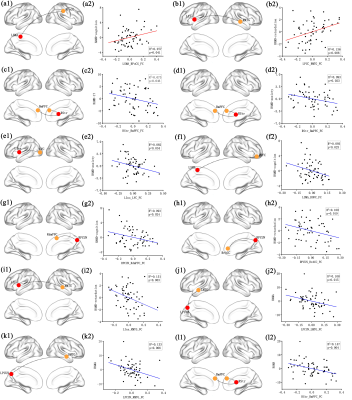
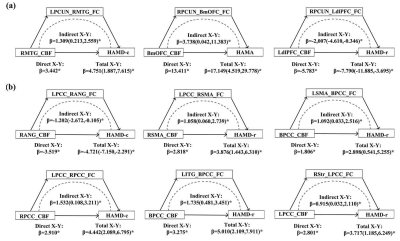
RESULTS: The CBF was significantly increased in MDDSI patients in the bilateral precuneus compared to HC and MDDNSI subjects. MDDSI patients exhibited enhanced FC in the prefrontal-limbic system and decreased FC in the right precentral gyrus relative to MDDNSI patients. Significant correlations were found between CBF, FC with clinical variables. More importantly, exploratory mediation analyses identified that the abnormal FC could mediate the association between regional CBF and behavioral performance in the MDD subgroup patients, separately.
DISCUSSION: First, ASL-derived CBF may be useful to understand brain metabolic and function 1, which can offer metabolic energy consumptions and a more biologically specific correlation of neural activity 2. The DMN, which involves the precuneus/PCC, MPFC as well as in the parietal cortex, widely distributed across brain regions 3. It is well-documented that the precuneus is significantly associated with emotional processing and is an important region of episodic memory and self-reflection 4,5, thus,increased perfusion in precuneus may be closely related to SI in depressed patients.Second, given the neurovascular coupling hypothesis, altered CBF may be tightly coupled to significant FC changes in the brain 6. So, further understanding of such mechanism has been facilitated by the development of FC network analyses based on the altered CBF regions. Our findings are generally concordant with previous reports in populations with or without SI symptoms and indicate that integrative dysfunctions of prefrontal-limbic system may contribute to disturbances in suicidal related symptoms in MDD patients. Intriguingly, we also found that MDDSI patients showed a significant difference in FC between left visual cortex and right precentral gyrus when compared with the MDDNSI and HC groups. A growing number of studies have found that people with depression have a wide range of executive dysfunction, such as response inhibition and impulse control disorder. This precentral gyrus is engaged in the executive function of response inhibition 7, so that this area may have an important relationship for the pathogenic factors of suicide 8. In other words, people who fail in inhibitory control show a propensity for negative emotional response or suicidal 9. Overt SI is inextricably linked to precentral functional and cortical abnormalities in patients with MDD 10,11. In addition, the emotional response of SI patients can participate in the brain feedback on physical movement 12. Relevant studies also found that a higher SI in adolescents MDD patients showed a relatively slow response in the postcentral gyrus (sensory perception) and the precentral gyrus (motor activity) 13, which is consistent with our results. Jointly, these evidence provide cues and information about SI neural circuits and support our hypotheses that the disrupted FC in prefrontal-limbic system and right precentral gyrus may play a crucial part in the vulnerability for SI patients. Third, the mediation analyses suggested that CBF-based FC could regulate the relationship between CBF and depression severity. The precuneus-mediated FC was found to be a mediator of the relationship between perfusion and HAMD-cognition, retardation traits, as well as HAMA in MDDNSI patients, while the PCC is more prominent in MDDSI patients. The decreased precuneus-mediated FC contributes to corresponding brain activity, resulting in higher HAMD-cognition, retardation traits, as well as HAMA levels. PCC is involved in emotional regulation, episodic memory and cognitive functions, and its abnormalities may affect cognitive and emotional problems 14. It exerts neural effects in cognitive impairment and delay, which was different from the results of MDDNSI group, suggesting that PCC is more closely involvement in process of SI. These results show that both perfusion and its functional coupling directly index behavioral scores, and expand our understanding of the relationship between CBF, FC and behavioral performance. However, this complex relationship is rarely explored and still needs further investigation.
CONCLUSION: These prominent results highlight the potential role of prefrontal-limbic system and precuneus gyrus in the process of suicide and provide new insight of neural mechanism underlying suicide in MDD patients.
Acknowledgements
We would like to thank all our participants, without whom this research would not have been possible to accomplish.References
REFERENCES:
1. de la Torre JC. Cerebral hemodynamics and vascular risk factors: setting the stage for Alzheimer's disease. J Alzheimers Dis. 2012;32:553-67.
2. Liu TT, Brown GG. Measurement of cerebral perfusion with arterial spin labeling: Part 1. Methods. J Int Neuropsychol Soc. 2007;13:517-25.
3. van Wingen GA, Tendolkar I, Urner M, et al. Short-term antidepressant administration reduces default mode and task-positive network connectivity in healthy individuals during rest. cc. 2014;88:47-53.
4. Amft M, Bzdok D, Laird AR, et al. Definition and characterization of an extended social-affective default network. Brain Struct Funct. 2015;220:1031-49.
5. Cavanna AE, Trimble MR. The precuneus: a review of its functional anatomy and behavioural correlates. Brain. 2006;129:564-83.
6. Wei Y, Wu L, Wang Y, et al. Disrupted Regional Cerebral Blood Flow and Functional Connectivity in Pontine Infarction: A Longitudinal MRI Study. Front Aging Neurosci. 2020;12:577899.
7. Tsujii N, Mikawa W, Tsujimoto E, et al. Reduced left precentral regional responses in patients with major depressive disorder and history of suicide attempts. PLoS One. 2017;12:e175249.
8. Bari A, Robbins TW. Inhibition and impulsivity: behavioral and neural basis of response control. Prog Neurobiol. 2013;108:44-79.
9. Mann JJ. Neurobiology of suicidal behaviour. Nat Rev Neurosci. 2003;4:819-28.
10. Hwang JP, Lee TW, Tsai SJ, et al. Cortical and subcortical abnormalities in late-onset depression with history of suicide attempts investigated with MRI and voxel-based morphometry. J Geriatr Psychiatry Neurol. 2010;23:171-84.
11. Sublette ME, Milak MS, Galfalvy HC, et al. Regional brain glucose uptake distinguishes suicide attempters from non-attempters in major depression. Arch Suicide Res. 2013;17:434-47.
12. Kragel PA, LaBar KS. Somatosensory Representations Link the Perception of Emotional Expressions and Sensory Experience. eNeuro. 2016;3:.
13. Nebel MB, Joel SE, Pekar JJ, et al. Disruption of functional organization within the primary motor cortex in children with autism. Hum Brain Mapp. 2014;35:567-80.
14. Fransson P, Marrelec G. The precuneus/posterior cingulate cortex plays a pivotal role in the default mode network: Evidence from a partial correlation network analysis. Neuroimage. 2008;42:1178-84.
Figures