3603
Radiation-induced structural network alterations in patients with nasopharyngeal carcinoma: a longitudinal study1School of Biomedical Engineering, Southern Medical University, Guangzhou, China, 2Department of Medical Imaging, Sun Yat-sen University Cancer Center, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Guangdong Key Laboratory of Nasopharyngeal Carcinoma Diagnosis and Therapy, Guangzhou, China, 3MR Research, GE Healthcare, Beijing, China
Synopsis
We conducted a longitudinal study to explore the radiation-induced alterations of structural brain network for nasopharyngeal carcinoma (NPC) patients using diffusion tensor imaging (DTI) technique and graph theory. The dose-dependent effect was also investigated using Spearman's Rank Correlation Coefficient. The structural brain connectivity was found to be altered at both 0~3 (acute) and 6 months (early-delayed) after radiotherapy (RT) and showed a tendency of recovery at 12 months (late-delayed) after RT. Also, the change of nodal properties were related to the temporal dose. These findings provide new insights into the pathophysiological mechanism of radiation-induced brain injuries.
Introduction
The radiotherapy (RT) is the main treatment for nasopharyngeal carcinoma (NPC) patients. However, the normal brain tissue surrounding the tumor is inevitably irradiated during cranial irradiation, causing brain structural abnormalities and cognitive decline. The mechanism of longitudinal evolution in brain injuries remains unclear. The study of how the structural brain network evolve over time after RT will facilitate the better understanding of RT-induced disorders, thereby aiding in diagnosis and treatment for NPC patients. A cross-sectional DTI study on three stages (before RT, 1-6 months and >6 months after RT) in NPC patients found that structural topological properties were altered within 1-6 months but began recovering >6 months after completing RT 1. Nevertheless, in cross-sectional study, the data at different stages were not from the same group and the cohort effect can compromise the ability to detect the RT-induced brain alteration. In this work, we adopt the prospective, longitudinal data to study the dynamic changes of structural brain network based on DTI probabilistic tractography and graph theory analysis for NPC patients.Methods
35 NPC patients (21 males; 23-60 years; 40.11±8.88 years) were enrolled. We repeatedly performed MRI scanning and neurocognitive tests at the following stages for each patient: before RT (baseline), 0~3 months (post-RT-AC), 6 months (post-RT-ED) and 12 months (post-RT-LD) after RT. The DTI data were acquired on a 3.0T GE scanner using SE-EPI sequence: TR/TE = 10000/63.8 ms, in-plane resolution = 2×2 mm2, slice thickness = 2 mm, 75 axial slices covering the whole brain, one volume with b=0 s/mm2, 30 volumes with b=1000 s/mm2.Data preprocessing includes the following steps: MPPCA denoising 2, eddy current and motion correction with an affine transformation, skull stripping with FSL-Brain Extraction Tool. The probabilistic tracking was performed with anatomically-constrained tractography 3, seeding from the interface between grey matter and white matter. Then, Spherical-deconvolution Informed Filtering of Tractograms (SIFT) 4 were performed to filter the streamlines from 10M to 1M. All the above preprocessing steps and fiber tracking were accomplished within MRtrix3.
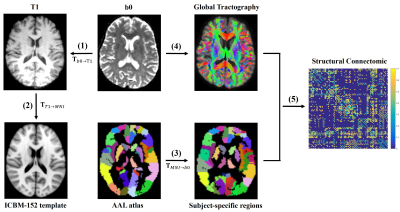
Figure 1 shows the flow chart of structural network construction. For each subject, the non-diffusion images were co-registered to the T1-weighted images with an affine transformation . Meanwhile, the T1-weighted images were nonlinearly transformed to the MNI space. The above two transformations were inverted and composed to wrap the automated anatomical labeling (AAL) 5 from MNI space to the native diffusion space of each subject. Finally, the 90 × 90 connectivity matrix for each subject was constructed.
Both the global and regional metrics were calculated to characterize the topological properties of altered structural network with GRETNA. The one-way repeated measures analysis of variance (ANOVA) was used and significance was set at p<0.05 with false discovery rate (FDR) correction for all statistical analyses. Spearman coefficient was calculated to investigate the relationship between the temporal nodal changes and irradiation dose.
Results
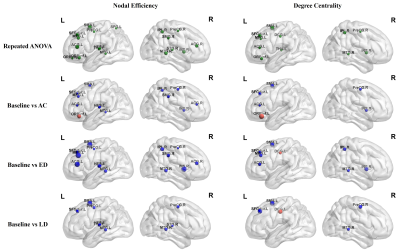
Figure 2 shows that the local efficiency significantly decreased at post-RT-ED and post-RT-LD compared to baseline with FDR corrected p value < 0.01. In addition, the local efficiency reached a largest decrease at post-RT-ED and showed a tendency of recovery at post-RT-LD.The significant alteration of the nodal efficiency (NE) and degree centrality (DC) among four stages was mainly located at the temporal, frontal, prefrontal, parietal and subcortical regions (Figure 3). Most of these altered regions exhibited a progressive decrease during post-RT-AC and post-RT-ED, and a partially or fully recovery at the post-RT-LD.
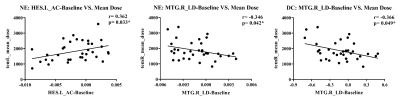
The decline of NE in the left heschl gyrus (HES.L) and right middle temporal gyrus (MTG.R), and the DC in the MTG.R were related to the mean temporal dose (Figure 4).
Discussion
The significant decrease of local efficiencies firstly occurred at 6 months after RT in our structural network study, later than the functional network alteration (<6 months) 6. This finding is reasonable because brain function might be more vulnerable or sensitive to attack 7. The “decrease-decrease-increase” pattern of nodal parameters may indicate that the structural brain reorganization mainly occurred in the late-delay stage which is generally consistent with previous studies 1,8-10.Conclusion
We used the follow-up data to monitor the dynamic changes of structural brain network after RT for NPC patients. The radiation-induced alterations of topological properties mainly began at the acute reaction stage and were aggravated at the early-delayed stage and then partially recovered at the late-delayed stage. The dynamic change patterns of topological properties facilitate a better understanding of potential mechanisms underlying radiation-induced brain injures. In addition, the dose-dependent alteration in the temporal regions (MTG.R and HES.L), indicating that these regions were more sensitive to dose and should be considered as part of radiotherapy treatment plan.Acknowledgements
This study was supported by the National Natural Science Foundation of China under Grant 61971214, the Natural Science Foundation of Guangdong Province under Grant 2019A1515011513, the Guangdong-Hong Kong-Macao Greater Bay Area Center for Brain Science and Brain-Inspired Intelligence Fund under Grant 2019022.References
1. Chen, Q., et al., Altered properties of brain white matter structural networks in patients with nasopharyngeal carcinoma after radiotherapy. Brain Imaging Behav, 2020. 14(6): p. 2745-2761.
2. Veraart, J., et al., Denoising of diffusion MRI using random matrix theory. Neuroimage, 2016. 142: p. 394-406.
3. Smith, R.E., et al., Anatomically-constrained tractography: Improved diffusion MRI streamlines tractography through effective use of anatomical information. NeuroImage, 2012. 62(3): p. 1924-1938.
4. Smith, R.E., et al., SIFT: Spherical-deconvolution informed filtering of tractograms. Neuroimage, 2013. 67: p. 298-312.
5. Tzourio-Mazoyer, N., et al., Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage, 2002. 15(1): p. 273-89.
6. Ding, Z., et al., Radiation-induced brain structural and functional abnormalities in presymptomatic phase and outcome prediction. Hum Brain Mapp, 2018. 39(1): p. 407-427.
7. Karim, H.T., et al., Intrinsic functional connectivity in late-life depression: trajectories over the course of pharmacotherapy in remitters and non-remitters. Mol Psychiatry, 2017. 22(3): p. 450-457.
8. Duan, F., et al., Whole-brain changes in white matter microstructure after radiotherapy for nasopharyngeal carcinoma: a diffusion tensor imaging study. Eur Arch Otorhinolaryngol, 2016. 273(12): p. 4453-4459.
9. Wang, H.Z., et al., Diffusion tensor imaging and 1H-MRS study on radiation-induced brain injury after nasopharyngeal carcinoma radiotherapy. Clin Radiol, 2012. 67(4): p. 340-5.
10. Xiong, W.F., et al., 1H-MR spectroscopy and diffusion tensor imaging of normal-appearing temporal white matter in patients with nasopharyngeal carcinoma after irradiation: initial experience. J Magn Reson Imaging, 2013. 37(1): p. 101-8.
Figures