3600
Preoperative high-resolution 3D VIBE evaluations of the neurovascular anatomy of patients with microvascular compression for hemifacial spasm1Departments of Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China, Wuhan,Hubei,China, China, 2Departments of Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan,Hubei,China, China, 3Philips Healthcare, Beijing, China, Beijing,China, China
Synopsis
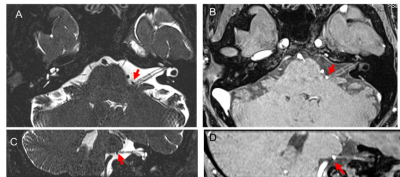
The main cause of hemifacial spasm is neurovascular compression syndrome. It is very important to preoperative evaluate the relationship between nerve and responsible blood vessel and its compression site. High-resolution 3D MR cisternography techniques were used preoperatively to assess neurovascular anatomy in patients with neurovascular compression syndrome, but the contrast between vessels and cranial nerves at the point of neurovascular contact is limited. In this study, we evaluated 3D VIBE image to could not only clearly show the structure of nerves and blood vessels, but also improve the contrast between blood vessels and nerves or surrounding brain stem.
Introduction
High-resolution 3D MR cisternography techniques such as 3D SPACE are used preoperatively to assess neurovascular anatomy in patients with neurovascular compression syndrome, but the contrast between vessels and cranial nerves at the point of neurovascular contact is limited. High-resolution 3D VIBE provides both high spatial resolution and excellent contrast in depicting the neurovascular contact[1-4]. We evaluated the usefulness of 3D VIBE in the evaluation of microvascular compression for hemifacial spasms compared with 3D SPACE and 3D TOF-MRA.MATERIALS AND METHODS
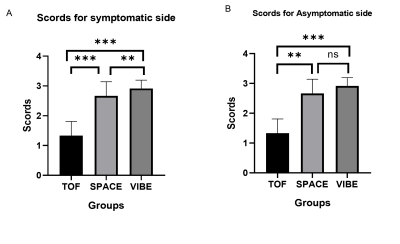
48 patients who underwent microvascular decompression for hemifacial spasm were examined preoperatively with 3D SPACE,3D TOF-MRA, and 3D VIBE. Two neuroradiologists retrospectively analyzed and scored lesion conspicuity, defined as the ease of discrimination between offending vessels and compressed nerves or the brain stem at the neurovascular contact. Comparative analysis of the image quality of the three groups to evaluate the neurovascular anatomy by a 4-point score. The kappa test was used to analyze the consistency of the two readers. The correlation between the degree of vascular compression and the clinical grade was analyzed by correlation analysis. The difference in image quality between the three methods was analyzed by the independent t-test. P <0.05 was considered to be a significant statistical difference.Results
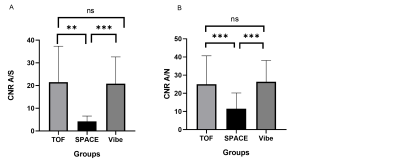
The ICC values in the interobserver analysis were 0.941, for qualitative analysis. The positive predictive value and specificity of the 3D VIBE image (95%,93.75%)were significantly higher than those of the 3D SPACE image (79%,78.3%) group (P <0.05). There was no significant difference between the two groups in sensitivity and negative predictive value (P> 0.05). The 3D VIBE image quality score (2.917 ±0.279) was significantly higher than that of 3D SPACE (2.667 ± 0.476) images and 3D TOF (1.333 ± 0.476) images, (P ≤ 0.01) on the symptomatic side. For the evaluation of the asymptomatic side, the score of the 3D VIBE image (2.979±0.144) was significantly higher than that of the 3D TOF group (1.167±0.429),while there was no significant difference between the 3D VIBE and 3D SPACE (2.896±0.309) scores (Figure 2). In quantitative analysis among three groups image quality by contrast-to-noise ratio. The contrast between blood vessels and brain stem in the 3D VIBE image (20.49±11.52) was significantly higher than those in the 3D SPACE image (4.21±2.37, p<0.05) but lower than that in the 3D TOF image(22.24±15.59). The contrast between blood vessels and nerves in the 3D VIBE image (26.33±11.492) was significantly higher than the 3D SPACE image (11.62±8.542, p<0.01, Figure 3). The clinical grade of hemifacial spasm was not significantly correlated with the degree of facial nerve compression (r = 0.26).Conclusion
High-resolution 3D VIBE is useful to evaluate neurovascular anatomy and to improve contrast in patients with microvascular compression for hemifacial spasm.Keywords
Neurovascular compression; Microvascular decompression; Hemifacial Spasm; High-resolution Magnetic resonance imageAcknowledgements
Many thanks to MR Collaborations, Philips Healthcare, Beijing, China.Many thanks to Department of Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology.References
1. Masuda Y, Yamamoto T, Akutsu H, Shiigai M, Masumoto T, Ishikawa E, Matsuda M, Matsumura A: Usefulness of Subtraction of 3D T2WI-DRIVE from Contrast-Enhanced 3D T1WI: Preoperative Evaluations of the Neurovascular Anatomy of Patients with Neurovascular Compression Syndrome. American Journal of Neuroradiology 2014, 36(2):317-322.
2. Öcal R, Tunç T, Ayas ZÖ, Yılmaz Ö, İnan LE: Comparison of brain MRI angiography and brain MRI cisternography in patients with hemifacial spasm. Acta Neurologica Belgica 2016.
3. Tanrikulu L, Scholz T, Nikoubashman O, Wiesmann M, Clusmann H: Preoperative MRI in neurovascular compression syndromes and its role for microsurgical considerations. Clinical Neurology and Neurosurgery 2015, 129:17-20.
4. Sekula RF, Frederickson AM, Branstetter BF, Oskin JE, Stevens DR, Zwagerman NT, Grandhi R, Hughes MA: Thin-slice T2 MRI imaging predicts vascular pathology in hemifacial spasm: A case-control study. Movement Disorders 2014, 29(10):1299-1303.
Figures