3598
Application of high-resolution 3D vessel wall MR(3D VW-MR) imaging in Primary Angiitis of the Central Nervous System1the First Hospital of Jilin University, Chang Chun, China, 2Philips Healthcare, Guangzhou, China
Synopsis
Primary angiitis of the central nervous system(PACNS) is a kind of rare disease, but the clinical diagnosis is difficult. Recently, high-resolution HR-3D-VW-MRI(3-dimensional vessel wall MR imaging) method has been used to evaluate cerebral vessels because it could directly show the vessel wall as well the lumen; thus it can assist in differentiating various types of vasculopathy. The purpose of our study was to summarize the typical imaging performance of PACNS and evaluate the value of 3D- VW-MRI sequence in demonstrating the detailed information in detection, diagnosis, evaluation, and follow-up for PACNS.
Purpose
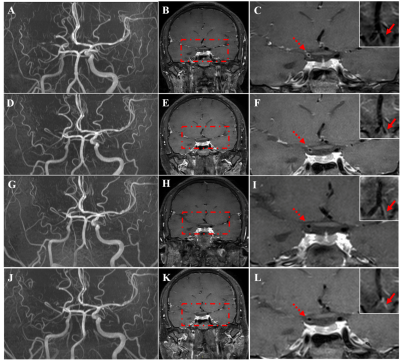
Vasculitis usually reveals a smooth, homogeneous, concentric arterial wall thickening and enhancement. To compare 3D vessel wall imaging with traditional magnetic resonance angiography (MRA) and provide valuable diagnostic information on PACNS from the perspective of radiography.Material and Methods
A total of seventeen patients(ten males and seven females) who were ultimately diagnosed with PACNS were recruited from March 2017 to March 2019 in the first hospital of Jilin University. 3DVW-MRI and MRA were performed on all patients. A 3D T1 VISTA(volume isotropic turbo spin-echo acquisition) protocol was performed on a 3.0T Ingenia MR Scanner (Philips Healthcare, Best, The Netherlands) with a standard 12-channel head/neck coil.The following parameters were used for the 3D T1 VISTA sequence:oblique coronal plane acquisition; variable refocusing flip angle; repetition time=350 ms; echo time=19 ms; field of view = 210 mm × 210 mm; acquired voxel size =0.8 mm × 0.8 mm × 0.8 mm; before and after intravenous gadolinium (0.1-0.2 mmol/Kg). A consecutive follow-up study was performed afterwards. Three cases with particular imaging characteristics on 3D VW-MRI were explored in this study, providing some hints on the application of 3D VW-MRI in PACNSResults
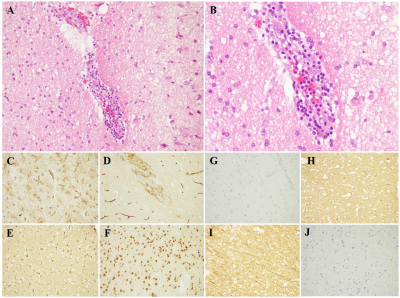
Seventeen cases of PACNS patients were recruited. The age ranges from 10 years old to 48 years old, with a median age of 32 years old. There were 12 cases (70.6%) combined with subcortical white matter involvement, 6 cases (35.3%) combined with the meningeal involvement, 2 cases (11.8%) complicated with basal ganglia involvement and 2 cases (11.8%) complicated with spinal cord involvement. Most of the lesions were with blurry border (16 cases,94.1%) , 2 cases (11.8%) were with clear border. Cortical atrophy was identified in 6 cases (17.6%). There were 12 cases (70.6%) with the enhancement of the lesions and meningeal. All the patients underwent routine head MRI, MRA, and 3D-VW-MRI. The 3D Vessel Wall MR imaging showed uniform thickness in all patients (100%) with contrast enhancement of the vessel wall of the vasculitis artery(Figure 1 and Figure 2). Imaging findings could be seen(Table 1). The brain pathology in 3 cases, manifested as brain tissue edema, partial degeneration and necrosis or brain tissue loose, blood vessel wall thickening and perivascular lymphocytes(Fig 3).Discussion
PACNS has three different pathology types: granulomatous, lymphocytic, and necrotizing vasculitis[1,2]. Among these, granulomatous vasculitis is the most common one, characterized by vasculocentric mononuclear inflammation and well-formed granulomas with multinucleated giant cells. VW-MRI can be used to directly visualize the abnormality of vessel wall; therefore, it has become an important tool for evaluation. Vasculitis is usually characterized by smooth, homogeneous, and concentric arterial wall thickening with enhancement, while atherosclerotic plaque usually displays nonconcentric and heterogeneous vessel wall abnormalities. In this study, 17 cases with PACNS were included. Among them 28 vessels were affected, inferring that cervical arteries were more vulnerable in PACNS. Both the long-axis and short-axis planes were analyzed for a precise interpretion of VW-MRI images. However, the 2D VW-MRI sequences could only be fixed at one short or long plane at a time. As the intracranial vessels can be quite oblique, curved, and tortuous, 2D sequences can lead to partial volume averaging effects and confound with vasculopathies[3]. As 3D VW-MRI is an isotropic sequence, it can apply reconstruction in any angle and reveal the head and neck vasculature in a relatively shorter time. 3D sequences can achieve relatively higher quality images than 2D sequences, because they are more stable against laminar flow and other artifacts.The vessel with post-processing techniques can be straightened because the slice thickness is only 1 mm. And for the images acquired during follow-up, the stenosis had not reverted; However its enhancement intensity had been gradually declined.Conclusion
3D-VW-MRI is now an optimal approach having obvious advantages over traditional angiographic methods. Firstly, it provides a good visualization of vessel wall and the lumen especially after the contrast agents. Second, as the thickness is only 1mm, thin enough with isotropic sequence, MPR(multi plannar reconstruction) and CPR(curved plannar reconstruction) in any angle are helpful for demonstrating the specific vasculopathy and the whole-brain vasculature. 3D-VW-MRI showed uniform thickness of the involved vessel. Furthermore, according to the enhancement intensity after contrast, the progression of PACNS could be evaluated. In conclusion, 3D-VW-MRI provides a more comprehensive information for detecting and diagnosing PACNS compared with the traditional methods.Acknowledgements
No acknowledgement found.References
1. Mandell DM, Matouk CC, FarbRI, et al. Vessel wall MRI to differentiate between reversible cerebral vasoconstriction syndrome and central nervous system vasculitis: preliminary results. Stroke 2012;43(3):860-2
2. Obusez EC, Hui F, Hajj-Ali RA, et al. High-resolution MRI vessel wall imaging: spatial and temporal patterns of reversible cerebral vasoconstriction syndrome and central nervous system vasculitis. AJNR American journal of neuroradiology 2014;35(8):1527-32
3. Mossa-Basha M, Hwang WD, De Havenon A, et al. Multicontrast high-resolution vessel wall magnetic resonance imaging and its value in differentiating intracranial vasculopathic processes. Stroke 2015;46(6):1567-73
Figures
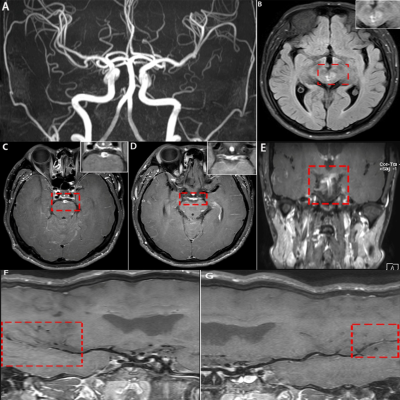
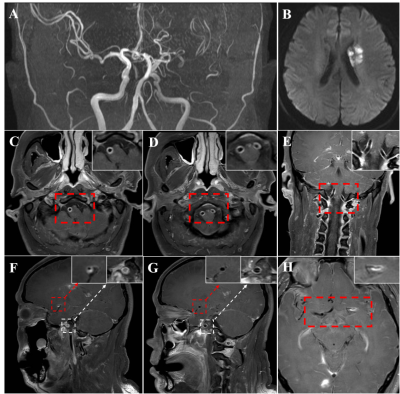
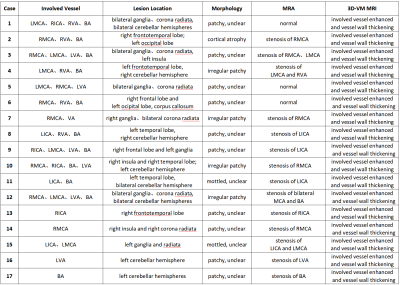
Table1 Imaging findings of primary central nervous system vasculitis
LMCA: left middle cerebral artery; LMCA: left middle cerebral artery; RICA: right internal carotid artery; RMCA: right middle cerebral artery; RV: right vertebral artery; LV: left vertebral artery; BA: basilar artery; SWI: susceptibility weighted imaging