3402
Bilateral characterization of fractional anisotropy within the anterior cruciate ligament: A step toward clinical use of DTI in the knee1School of Medicine, Queen's University, Kingston, ON, Canada, 2Department of Orthopedic Surgery, Queen's University, Kingston, ON, Canada, 3Center for Neuroscience Studies, Queen's University, Kingston, ON, Canada, 4Department of Orthopedic Surgery, McGill University, Montréal, QC, Canada
Synopsis
Diffusion tensor imaging (DTI) has emerged as biomarker to characterize the ligamentization process of the anterior cruciate ligament (ACL), following surgical reconstruction. One major limitation to this approach is the necessity for pre-injury baseline measurements to be used as a frame of reference, in order to inform clinical decision making with respect to recovery of the graft, and return-to-activity (RTA). Here, we explore the linear relationship for anisotropy between knees bilaterally, in healthy participants, to provide a methodological framework that allows for the clinical integration of DTI to monitor recovery of the tendon autograft, following surgical reconstruction, and inform RTA.
INTRODUCTION
Reconstruction of the anterior cruciate ligament (ACL) is the preferred management for most patients with complete ACL rupture, in order to achieve rotational and translational stability, and facilitate the return to activity (RTA). Although it is understood that the tendon autograft undergoes a transition from a tendinous to ligamentous composition postoperatively 1,2, knowledge about the longitudinal microstructural changes in tissue integrity of the autograft post-ACL reconstruction remains limited.Diffusion tensor imaging (DTI) has emerged as an objective quantitative marker to characterize the ligamentization process of the tendon autograft following surgical reconstruction3-7. Clinically, DTI has been associated with the degree of ligamentous injury 3, while showing promise as a tool to monitor tissues recover following surgical reconstruction of the ACL4. One major limitation to this approach is the necessity for pre-injury baseline measurements to be used in order to inform clinical decision making with respect to recovery of the graft, and RTA. Here, we explore the linear relationship for anisotropy (fractional anisotropy, FA) between knees bilaterally, in healthy participants, with the hypothesis that good agreement between a patient’s knees may provide a methodological framework allowing for the clinical integration of DTI to monitor recovery of the tendon graft, following surgical reconstruction and inform RTA.
METHODS
Ten healthy participants with no previous history of knee injuries were consented to participate in this study (age, 26 ± 2 years; M/F, 4/6). All images were acquired on a Magnetom Prisma Siemens scanner at 3.0T, using a secured flexible 18-channel body coil wrapped around the knee (Figure 1). Both knees were scanned for each participant enrolled in the study.A 3D anatomical Double Echo Steady State (DESS) sequence with isotropic resolution (8.35 min; in-plane resolution, 0.2 x 0.2 mm ; slice thickness, 0.4 mm; TR/TE, 14.16/5.00 ms; Partial Fourier, 7/8) was acquired (Figure 2) on which regions of interest (ROI) were placed consistent with the end points of the ACL (femur, posteromedial corner on medial aspect of lateral condyle; tibia, anteromedial to intercondylar eminence; Figure 2). Diffusion images were acquired using the following parameters, fat saturation and anterior-posterior phase encoring directions 8,9: 0.42 min; in-plane resolution, 1.5 x 1.5 mm; slice thickness, 3 mm; TR/TE, 1300/45 ms; b-values, 0, 400 s/mm2; Partial Fourier, 6/8; GRAPPA factor, 2. The diffusion sequence was repeated 10 times to improve signal-to-noise ratio. Five additional B0 maps with reversed phase encoring direction (i.e., posterior-anterior) were also acquired to optimize distortion corrections.
All diffusion images were processed using the FMRIB FSL toolbox10. Transformation matrices co-registering the averaged B0 image to the high-resolution anatomical image were inverted to align the ROIs for fiber-based probabilistic tractography (FBPT), into native diffusion space. Following Bayesian modelling of crossing fibers 11,12, the ACL was reconstructed using FBPT, which was repeated twice using each spherical ROI as the seed, or the target. The final tractography-based ACL mask was constructed using voxels traveled by both tractograms.
Average FA was computed for each subject, in both knees, and then correlated against one another using a Pearson correlation (testing for normality, P > 0.05), to assess the degree of similarity in anisotropy between the ACLs. Statistical significance was set to P < 0.05. This was repeated for a manually delineated segmentation of the ACL, for direct comparison of the segmentation method. The manual segmentation was restricted to the ACL contained within the ROI seeds, in order to align with the spatial restrictions applied to the FBPT.
RESULTS
A total of 20 datasets were collected for this study (1/knee/participant; N=10). Successful reconstruction of the FBPT-ACL was accomplished in all participants. The group average FA (± standard deviation) for the manually segmented ACL mask, as well as the FBPT mask, were found to equal 0.1840 ± 0.0190 (manual, dominant leg) and 0.1954 ± 0.0276 (manual, non-dominant leg), and 0.1647 ± 0.0243 (FBPT, dominant leg) and 0.1681 ± 0.0257 (FBPT, non-dominant leg), respectively.When comparing both knees, within patients, better agreement was found for the FBPT-derived ACL mask, in comparison to the manual segmentation (Figure 3). Specifically, the linear correlation coefficient for the FBPT-derived ACL mask was found to equal 0.88, while only reaching a sub-optimal value of 0.54 for the manually segmented mask.
DISCUSSION/CONCLUSION
We sought to assess the degree of concordance in FA between the left and right knee, in healthy participants, as way to provide insight toward using a contralateral “healthy” knee for a patient undergoing ACL reconstruction as a reference for the recovery of the tendon autograft. Good agreement in anisotropy can be achieved between the left and right knee, especially if the FBPT method is used for semi-automated segmentation of the ACL, which is likely a result of removing inherent bias and inconsistencies associated with drawing the ligamentous structure across scans/patients.These findings suggest that contralateral anisotropy of the ACL, assuming no previous injuries, may be used as a quantitative reference biomarker for monitoring the recovery of the tendon autograft following surgical reconstruction. Clinically, this may be used as an index to supplement decision-making with respect to RTA, as well as reducing rates of re-injuries.
Acknowledgements
AAC would like to acknowledge funding from the PSI Foundation (ON, Canada) Research Trainee grant, as well as funding from the Department of Surgery at Queen's University (Kingston, ON, Canada). AAC would also like to acknowledge funding and support from the Center for Neuroscience studies at Queen's University (Kingston, ON, Canada).References
1. Amiel D, Kleiner JB, Roux RD, Harwood FL, Akeson WH. The phenomenon of "ligamentization": anterior cruciate ligament reconstruction with autogenous patellar tendon. J Orthop Res. 1986;4(2):162-172.
2. Janssen RP, Scheffler SU. Intra-articular remodelling of hamstring tendon grafts after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22(9):2102-2108.
3. Liu S, Liu J, Chen W, et al. Diffusion Tensor Imaging for Quantitative Assessment of Anterior Cruciate Ligament Injury Grades and Graft. J Magn Reson Imaging. 2020;52(5):1475-1484.
4. Van Dyck P, Billiet T, Desbuquoit D, et al. Diffusion tensor imaging of the anterior cruciate ligament graft following reconstruction: a longitudinal study. Eur Radiol. 2020;30(12):6673-6684.
5. Van Dyck P, Froeling M, De Smet E, et al. Diffusion tensor imaging of the anterior cruciate ligament graft. J Magn Reson Imaging. 2017;46(5):1423-1432.
6. Yang X, Chen D, Li M, Shi D, Zhu B, Jiang Q. Diffusion tensor imaging of the anterior cruciate ligament graft after reconstruction: repeatability and diffusion tensor imaging metrics. J Comput Assist Tomogr. 2015;39(2):244-249.
7. Yang X, Li M, Chen D, et al. Diffusion tensor imaging for anatomical and quantitative evaluation of the anterior cruciate ligament and ACL grafts: a preliminary study. J Comput Assist Tomogr. 2014;38(4):489-494.
8. Champagne A, Brien D, McGuire A, et al. Optimizing the use of diffusion tensor imaging for clinical tractography of the anterior cruciate ligament in the knee. ISMRM; 2021; Vancouver, BC, Canada.
9. Griswold MA, Jakob PM, Heidemann RM, et al. Generalized autocalibrating partially parallel acquisitions (GRAPPA). Magn Reson Med. 2002;47(6):1202-1210.
10. Jenkinson M, Beckmann CF, Behrens TE, Woolrich MW, Smith SM. Fsl. Neuroimage. 2012;62(2):782-790.
11. Jbabdi S, Sotiropoulos SN, Savio AM, Grana M, Behrens TE. Model-based analysis of multishell diffusion MR data for tractography: how to get over fitting problems. Magn Reson Med. 2012;68(6):1846-1855.
12. Behrens TE, Woolrich MW, Jenkinson M, et al. Characterization and propagation of uncertainty in diffusion-weighted MR imaging. Magn Reson Med. 2003;50(5):1077-1088.
Figures
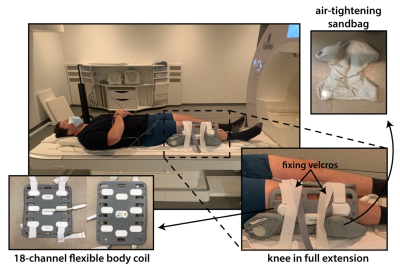
Figure 1. Set-up for MRI of the knee
Participants were placed supine with their knee in 10° of flexion. An 18-channel flexible body coil was wrapped around the participant’s knee, which was then secured using an air-tightened sandbag. Velcros were used to anchor the apparatus to the MR-compatible bed in order to minimize motion.
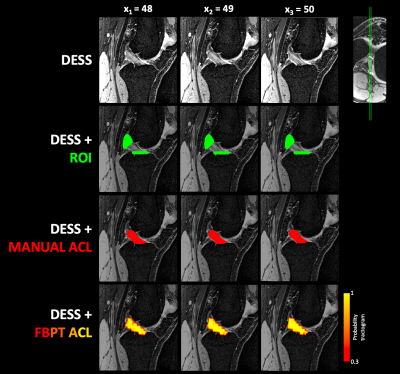
Figure 2. Diffusion tensor imaging of the anterior cruciate ligament (left knee)
Three sagittal views of the Double Echo Steady State (DESS) scan are shown highlighting the anterior cruciate ligament (ACL). The matching slices in the second row show the region of interest (ROI) seeds/target placed within the tibia and femur insertions of the ACL (green). The third and fourth rows show the manual segmentation of the ligament (red) and the fiber-based probabilistic tractography (FBTP) results (red-yellow), which were both contained with the pre-determined ROI seeds/target.
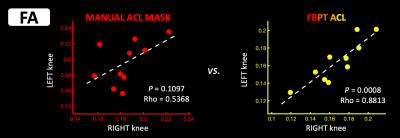
Figure 3. Linear relationship for mean fractional anisotropy (FA) between the left and right knees in healthy control participants
The mean FA was computed for the manually segmented anterior cruciate ligament (ACL), as well as the mask generated using fiber-based probabilistic tractography (FBPT). A least-square best fit line was plotted (white, dotted) for each dataset.