3375
Feasibility of VDP Calculation using 19F Free Breathing Spiral Acquisition with Post-Acquisition Denoising1Biomedical Engineering, University of North Carolina, Chapel hill, NC, United States, 2Department of Radiology, Case Western Reserve University, Cleveland, OH, United States, 3Department of Radiology and Biomedical Research Imaging Center, University of North Carolina, Chapel hill, NC, United States, 4Division of Pulmonary and Critical Care Medicine, University of North Carolina, Chapel hill, NC, United States, 5Marsico Lung Institute/UNC Cystic Fibrosis Center, University of North Carolina, Chapel hill, NC, United States, 6Division of Pediatric Pulmonology, University of North Carolina, Chapel hill, NC, United States
Synopsis
19F lung ventilation MRI is usually acquired with extended breath holds that limit the acquisition to relatively healthy patients. New denoising methods have the potential to decrease the scan time significantly while achieving comparable SNRs. We compare 19F breath held scans to spiral acquisition based scans performed while free breathing combined with post-acquisition denoising in human subjects at 3T. VDP and SNR were evaluated. The denoised spiral scans yield higher SNRs (29.3 average increase) but overestimated VDPs (8.5% average increase). The differences in VDP were correlated (R-squared 0.74). The approach shows the potential for free-breathing 19F MRI ventilation imaging.
Introduction
19F ventilation MRI with fluorinated gases has been previously shown to be effective at lung disease stage characterization in both CF and COPD patients1,2. The 19F gases, including perfluororpropane and SF6 are mixable with oxygen for creating normoxic gas mixtures for patients. This approach has the potential of measuring lung function spatially3, without the need for ionizing radiation.Though hyperpolarized gas approaches offer greater signal, no hyperpolarizer is needed for 19F imaging. However, one major limitation of 19F MRI with conventional sequences is the scan time required to achieve adequate SNR, as most acquisitions are performed at breath-holds with an acquisition time of 8 to 16 seconds1,2 and as short as 2.12 to 5.624 seconds. This limitation constraints 19F lung imaging to patients able to follow commands and relatively healthy patients.
A shorter acquisition time could enable the application of 19F lung MRI to patients unable to hold their breath and for pediatric use. In this study we explore the feasibility of the combination of spiral acquisition and post-acquisition denoising. Our method is compared to our previously reported acquisition approach with breath holds1. VDP and SNR values are used as comparison metrics.
Methods
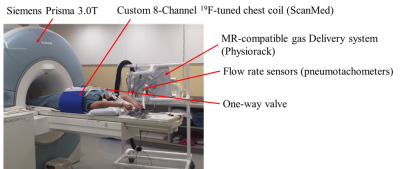
Five subjects with CF were recruited and underwent 19F lung MR imaging in a multinuclear capable Siemens Prisma 3.0T scanner (Siemens Medical Systems, Erlangen, Germany) and a custom 8-channel 19F-tuned chest coil (ScanMed, Inc., Omaha NE). The patients breathed a normoxic mixture of 79% PFP and 21% O2 (Air Liquide Healthcare, Plumsteadville, PA). For the wash-in portion, patients breathed in the mixture starting with a tidal volume inspiration-expiration cycle followed by a maximal inspiration and breath-hold. During the breath hold lasting 12 seconds, a 3D GRE sequence (FA 74°, TE 1.61 ms, TR 13 ms, 15 mm slice thickness, and a 64 by 64 acquisition matrix with a 130 Hz/pixel bandwidth and an in-plane resolution of 6.25 mm x 6.25 mm) was performed, once the acquisition ended, the patient was instructed to breath out and start the next cycle with a tidal inspiration. 5 cycles were performed for the wash-in portion resulting in 5 breath hold acquisitions. More details of the method can be found in1.In between the breath holds, a 12 repetition 4 arms spiral sequence tuned to 19F was allowed to run while the patient was free breathing, each repetition lasted 0.45 seconds with TR 11ms, TE 0.48ms, resolution and slices were identical to the breath hold acquisition. The wash-out portion was similar to the wash-in portion but the patient inhaled room air and lasted for 8 cycles or until no visible 19F signal was present. Additionally, 1H MRI GRE VIBE images were acquired during a 15 second maximal inspiration breath hold (FA 5°, TR 2.42 ms, TE 0.05 ms, 224 by 224 acquisition matrix, and resolution of 2.1 mm x 2.1 mm x 2.5 mm). The 5th breath hold acquisition and its corresponding spiral acquisition were used to measure SNR and VDP reported in this study. The spiral acquisitions were denoised using a previously published method in the complex domain6. The anatomical scans were registered to the 19F scans and masks were drawn to cover the whole thoracic lung cavity. VDP was measured as regions in the lung with signal lower than the 95th percentile signal intensity of the most posterior slice which lies outside the lungs and therefore contains only noise in the 19F scans. SNR was calculated as the ratio between the mean signal inside the lung at the highest signal coronal slice over the standard deviation of the most posterior slice values.Results
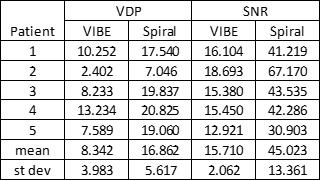
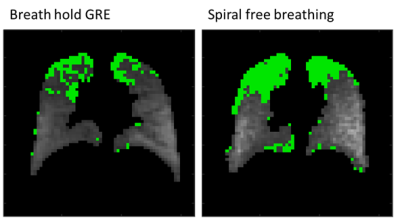
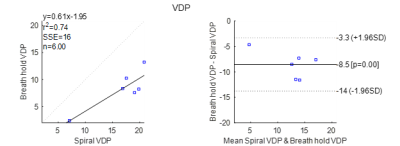
Denoising successfully increased the SNR of 19F signal in all patients by 29.3 in average, however, the VDP also increased by 8.5% in average. Table 1 shows the VDP and SNR results for all 5 patients and the mean and standard deviations. Figure 3 shows an example coronal slice comparing VDP from breath hold GRE and free breathing spiral. The increase in VDP by the spiral method was observed to increase and correlate with the breath hold VDP with a R-squared score of 0.74. Potential sources of error are the differences in lung inflation between maximum inhalation breath holding and free breathing, another potential source of error is the difference in sensitivity of the two compared acquisition methods.Conclusion
Using a spiral 19F MRI combined with denoising has been shown to increase SNR substantially, the short time of acquisition (0.45 seconds) allows for free breathing acquisition. VDP calculated from free breathing spiral is overestimated but correlated (R-squared 0.74) to the VDP calculated from the longer breath hold 19F GRE acquisition.Acknowledgements
This work was supported by the Cystic Fibrosis Foundation (DONALD14XX0 and GORALS19Y5) and the NIDDK (P30 DK 065988 and DK 108231).References
1. Goralski, Jennifer L., et al. "Dynamic perfluorinated gas MRI reveals abnormal ventilation despite normal FEV1 in cystic fibrosis." JCI insight 5.2 (2020). 2.
2. Gutberlet, Marcel, et al. "Free-breathing dynamic 19F gas MR imaging for mapping of regional lung ventilation in patients with COPD." Radiology 286.3 (2018): 1040-1051. 3.
3. Couch, Marcus J., et al. "Pulmonary ultrashort echo time 19F MR imaging with inhaled fluorinated gas mixtures in healthy volunteers: feasibility." Radiology 269.3 (2013): 903-909. 4.
4. Charles HC, Jones RW, Halaweish AF, Ainslie MD. Parallel Imaging for Short Breath Hold Times in Perfluorinated Gas Imaging of the Lung. Proc Intl Soc Mag Reson Med 23. 2015;23:3984. 5.
5. H. C. Charles and B. J. Soher, “Systems, methods, compositions and devices for in vivo magnetic resonance imaging of lungs using perfluorinated gas mixtures,” US9724015 B2, 08-Aug-2017 6.
6. Huynh, Khoi Minh, et al. "Noise Mapping and Removal in Complex-Valued Multi-Channel MRI via Optimal Shrinkage of Singular Values." International Conference on Medical Image Computing and Computer-Assisted Intervention. Springer, Cham, 2021.
Figures