3359
Are vascular risk factors associated with white matter health equally between men and women?1Rotman Research Institute, Baycrest Health Sciences, Toronto, ON, Canada, 2Department of Medical Biophysics, University of Toronto, Toronto, ON, Canada
Synopsis
White matter microstructural degeneration is an early marker of declining brain health, and vascular risk factors such as high blood pressure and adipose fat deposition have been found to be significantly associated with white matter microstructural degeneration in healthy adults. In this study, using diffusion tensor imaging, we find that the vascular-risk influences on white matter are more pronounced in women than in men. This study therefore calls attention to the consideration of sex differences in studying brain vulnerability to vascular risk factors.
Introduction
High abdominal fat and blood pressure are interrelated vascular risk factors[1] and contribute to pathological aging, such as the development of type 2 diabetes[2]. Previous literature has found associations of both blood pressure (BP) and adiposity with human white matter microstructure by using metrics derived from diffusion tensor imaging (DTI). Blood pressure and adiposity have been shown to be negatively correlated with FA and AD and positively correlated with MD and RD in regions including the corpus callosum[3-9], fronto-occipital fasciculi[4-5,10], fornix[8,10], corona radiata[9], cingulum[10], and cerebellar peduncles[9]. One study of body-mass-index (BMI) found significantly lower AD among both males and females with higher BMI in the corpus callosum, but only significantly higher RD among females with higher BMI[6], which suggests a sex-dependence. Previous studies have also theorized a link between the expression of female hormones such as estrogen and a higher predisposition towards abdominal obesity, placing females at higher risk for white matter degeneration[11]. However, existing studies on the sex-dependence of these associations are limited in sample size and methodological rigor. Given these theorized sex differences, the present study seeks to explore the sex-dependence of associations of blood pressure and abdominal fat with the various DTI metrics.Methods
All data were taken from the UK Biobank. Subjects were excluded from our study if they reported a neurological, psychological or psychiatric disorder, neurological injury, or history of stroke. The sample consisted of 281 subjects aged 46-79 (158 male). Diffusion MRI data were acquired as part of the UK Biobank on a Siemens Skyra 3T system with 5 b=0 and 50 b=1000s/mm2 at TR = 3.6s, TE=92ms, matrix size=104x104x72 with (2mm)3 resolution, 6/8 partial Fourier, 3x multislice acceleration and no in-plane acceleration. An additional 3 b=0 volumes were acquired with a reversed phase encoding. The data were corrected for eddy-current and susceptibility-related distortions via EDDY and TOPUP respectively.FSL’s TBSS was used to obtain a WM skeleton. For voxelwise analysis, an effect was computed using a linear model defined by p<0.05 with correction for multiple comparisons (cluster-wise controlling family-wise error rate with 5000 permutations) and controlling for age as per FSL’s randomise.
The following DTI metrics were used in analyses: FA, MD, AD and RD. Each DTI metric was investigated for positive and negative associations with either SBP or AFR. This was done without controlling for sex or age, controlling for only sex, and controlling for both sex and age. Age was controlled to account for SBP/AFR and white matter microstructure both being strongly correlated with age.
In addition, a comparison of the associations between either SBP or AFR and the DTI metrics was conducted for males and females. This was conducted without controlling for age, and while controlling for age to account for age-related changes in white-matter microstructure.
Results
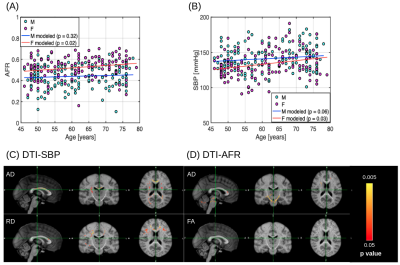
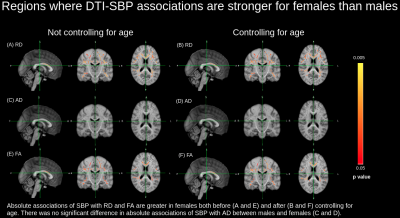
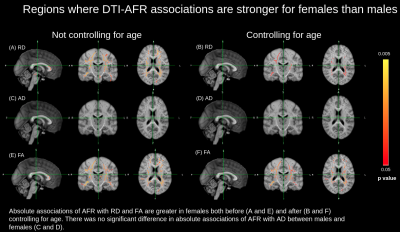
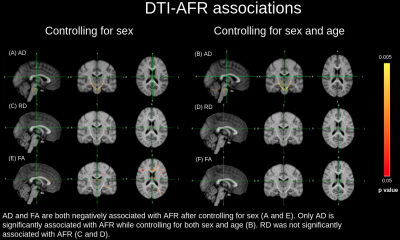
SBP and AFR were significantly, positively correlated with age in females only. No significant correlation between SBP or AFR and age was observed for males (Figure 1a and 1b). In general, AD and RD were positively associated with SBP (Figure 1c). Meanwhile, AD and FA were negatively associated with AFR (Figure 1d).The sex-dependent effects of blood pressure (SBP) and abdominal fat ratio (AFR) were found to vary by DTI metric. The strength of associations between SBP with RD and FA were significantly greater in females compared to males (Figure 2). Furthermore, strength of associations between AFR with RD and FA were significantly greater in females compared to males (Figure 3). With the exception of the AFR-RD associations, regional differences for males and females remained consistent when controlled for age. Of note, no significant sex differences were observed for the AD-SBP or AD-AFR associations.
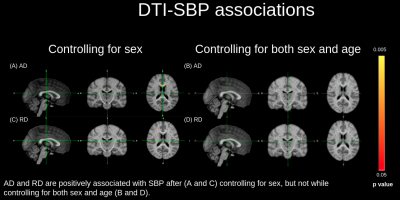
In addition, AD and RD were positively associated with SBP, both with and without controlling for sex, but not while controlling for both sex and age (Figure 4). Likewise, AD and FA were negatively associated with AFR with and without controlling for sex, but not while controlling for both sex and age (Figure 5).
Discussion and Conclusion
Significant differences in the associations of SBP and AFR with the DTI metrics in males and females suggests that the effects of SBP and AFR on white matter health may be sex-dependent.Given that the differences persisted when controlling for age, it may be that aging enhances these sex differences in SBP/AFR and white matter associations. An alternative explanation is that aging has different effects on males and females, and that these differences exist independently of age effects. Based on these differences, future studies investigating blood pressure, body fat and white matter health should account for sex differences for their analyses.
Lastly, extensive literature exists which links body fat and hypertension to cognitive deficits such as those affecting memory and executive function[12]. Lower white matter microstructural integrity in regions such as the anterior limb of the internal capsule, fornix, superior longitudinal fasciculus and superior corona radiata have previously been associated with reduced executive function[13]. Therefore, future studies should also explore whether sex differences in those associations align with the sex differences observed in this study.
Acknowledgements
This research has been conducted using the UK Biobank Resource under Application Number 40922. We thank CIHR for financial support.References
1. Sironi et al (2004) Visceral fat in hypertension: influence on insulin resistance and beta-cell function. Hypertension. 44:127-33.
2. Nordström et al (2016) Higher Prevalence of Type 2 Diabetes in Men Than in Women Is Associated With Differences in Visceral Fat Mass. J Clin Endocrinol Metab. 101: 3740–3746.
3. Allen et al (2016) Higher Blood Pressure Partially Links Greater Adiposity to Reduced Brain White Matter Integrity. Am J Hypertens. 29:1029-1037.
4. Karlsson et al (2013) Obesity is associated with white matter atrophy: a combined diffusion tensor imaging and voxel-based morphometric study. Obesity (Silver Spring). 21:2530–2537.
5. Maillard et al (2012) Effects of systolic blood pressure on white-matter integrity in young adults in the Framingham Heart Study: a cross-sectional study. Lancet Neurol. 11:1039–1047.
6. Mueller et al (2011) Sex-dependent influences of obesity on cerebral white matter investigated by diffusion-tensor imaging. PloS one. 6:e18544.
7. Salat et al (2012) Inter-individual variation in blood pressure is associated with regional white matter integrity in generally healthy older adults. NeuroImage. 59:181–192.
8. Stanek et al (2011) Obesity is associated with reduced white matter integrity in otherwise healthy adults. Obesity (Silver Spring). 19:500–504.
9. Verstynen et al (2013) Competing physiological pathways link individual differences in weight and abdominal adiposity to white matter microstructure. NeuroImage. 79:129-137.
10. Hannawi et al (2018) Hypertension Is Associated with White Matter Disruption in Apparently Healthy Middle-Aged Individuals. AJNR Am. J. Neuroradiol. 39:2243–2248.
11. Mauvais-Jarvis (2015) Sex differences in metabolic homeostasis, diabetes, and obesity. Biol. Sex Differ. 6:14.
12. Elias et al (2003) Lower cognitive function in the presence of obesity and hypertension: the Framingham heart study. Int J Obes Relat Metab Disord. 27:260–268
13. Heidi et al (2013) Association between white matter microstructure, executive functions, and processing speed in older adults: the impact of vascular health. Hum Brain Mapp. 34:77-95
Figures