3289
Clinical DIADEM: Distortion-Free High-Resolution Diffusion-Weighted Imaging of the Brain.
Myung-Ho In1, Norbert G Campeau1, Joshua D Trzasko1, Daehun Kang1, Kirk M Welker1, John Huston III1, Yunhong Shu1, and Matt A Bernstein1
1Department of Radiology, Mayo Clinic, Rochester, MN, United States
1Department of Radiology, Mayo Clinic, Rochester, MN, United States
Synopsis
Echo-planar based diffusion-weighted imaging (DWI) of the brain is prone to local image distortion which can lead to misdiagnosis or nondiagnostic image quality in areas prone to susceptibility effects. A novel distortion-free imaging scheme, termed DIADEM (Distortion-free Imaging: A Double Encoding Method) was recently introduced and optimized for brain imaging on a high-performance experimental Compact 3T system. In this study, we fully implement the DIADEM DWI technique on two 510-k cleared, whole-body 3T scanners and explore the clinical feasibility for its use in routine clinical practice.
Introduction
Clinical diffusion-weighted imaging (DWI) is commonly based on echo-planar imaging (EPI) and suffers from susceptibility- and diffusion-gradient-direction-oriented eddy-current-induced image distortions, which often results in nondiagnostic image quality in local high susceptibility areas of the brain and potentially lead to misdiagnosis (e.g., a false negative or false positive result). Recent technical advances such as parallel imaging1, reduced FOV DWI2, and multi-shot approaches3,4 are improvements over routine EPI-based DWI, however, the degree of distortion remains prominent at 3T, especially in proximity to air-tissue interfaces. A novel distortion-free imaging scheme, termed DIADEM (Distortion-free Imaging: A Double Encoding Method) was recently introduced and optimized on a high-performance Compact 3T scanner5,6 and showed robust diffusion imaging in susceptibility prone regions. In this study, we implemented DIADEM-DWI on two clinical 3T scanners and further characterized its performance relative to conventional EPI-based DWI of the brain.Methods
Implementation of online DIADEM reconstruction: The flowchart of online DIADEM reconstruction pipeline is presented in Fig. 1. Due to its new imaging strategy that is not supported by vendor reconstruction, the automatic DIADEM reconstruction pipeline has been developed and is performed under MATLAB compiler runtime (MCR) environment on a secure external high-performance reconstruction server located outside the MRI network segment utilized with 16 multicore computing processors. All network communications are initiated scanner-side and utilize outbound communication pathways only to avoid any security issue – i.e., the server is incapable of initiating a connection to the scanner. Sequential reconstruction is conducted on the server to reconstruct all the DIADEM scans from multiple scanners. As provided in vendor EPI-DWI reconstruction, a trace (i.e., combined DW images) and apparent-diffusion-coefficient (ADC) map are also calculated in the DIADEM-DWI reconstruction.Feasibility study for routine clinical practice: DIADEM-DWI was first evaluated for clinical use on a commercially available (60 cm) whole-body 3T scanner with a gradient performance of 50 mT/m and 200 T/m/s (MR750, GE Healthcare) and a standard 8-channel coil (Invivo Corp). Under IRB-approved protocols, first ten patients scheduled for a clinical brain MRI exam with standard diffusion (i.e., EPI-DWI) were recruited to additionally obtain the DIADEM-DWI scan for comparison. Next, the comparison study was translated to a wide-bore (70 cm) 3T scanner with a lower gradient performance of 33 mT/m and 120 T/m/s (MR750W, GE Healthcare) using a 32-channel head coil (Nova Medical). Clinical EPI-DWI scan was obtained on both whole-body 3T scanners with following imaging protocols: FOV=220×220 mm2, matrix size (readout×phase-encoding)=128×256, image resolution=1.72×0.86, 38 slices, slice thickness=4 mm, one non-DW (i.e., T2) and three DW images with b=1000 mm2/s, and scan time=1:00~1:10. The identical protocols were applied in DIADEM-DWI scans on MR750/MR750W 3T scanners, except for the matrix size=220×120/200×200, image resolution=1×1.83/1.1×1.1 mm2, multiband=1/2, and scan time=4:00/3:59.
Results and Discussion
Strong local distortions are clearly visible in EPI-DWI near boundaries of temporal and frontal lobes on a clinical whole-body 3T scanner (Fig. 2). In distinction, negligible distortion was observed in DIADEM and the images matched very well to the geometrically correct reference (i.e., fast-spin-echo) image. Since this approach is immune to both T2* blurring and eddy-current-induced distortions varying according to the applied (i.e., three) diffusion directions, the images were visually much sharper than EPI even though the intrinsic image resolution in EPI was slightly higher (Fig. 2). In addition, additional magnetic susceptibility artifacts induced by metallic shunt components were effectively resolved in DIADEM imaging (Fig. 3). Compared to the standard EPI-DWI, DIADEM-DWI produced more reliable diffusivity coefficients, even in local brain structures with high susceptibility effects including internal auditory canal (Fig. 4A), cisternal segment of the trigeminal nerve (Fig. 4A), and optic nerve (Fig. 4B). Acquisition time for DIADEM-DWI was around 4 minutes compared to 1:10 minutes for EPI-based DWI, but still acceptable for clinical use. High image resolution on DIADEM was possible using multiband imaging7 on the wide-bore 3T scanners, even with the lower gradient performance MR750W scanner (Fig. 5). The reconstruction time including the data transfer time over network were around 7 and 15 minutes, respectively without and with multi-band imaging protocol, which could be further reduced by translating the MATLAB- to C-based reconstruction algorithm in future.DIADEM-DWI provided improved depiction and conspicuity of brain structures compared to standard EPI-DWI. DIADEM permitted more confident diagnosis of small acute brain infarctions in local high-susceptibility areas that are commonly challenging to interpret, primarily because of fewer artifact-related false positive and false negative results. Visualization of cranial nerves, orbital and suprahyoid neck structures was markedly improved with DIADEM. Evaluation of postoperative DWI changes was also superior with DIADEM-DWI due to reduced image degradation related to post-surgical susceptibility changes and areas of pneumocephalus.
Conclusion
DIADEM high-resolution distortion-free DWI was successfully implemented onto clinical 3T scanners and demonstrated marked improvements in diffusion signal characterization compared to the currently implemented EPI-based DWI, especially in local high-susceptibility regions.Acknowledgements
This work was supported by NIH U01 EB024450, NHI U01 EB026979, and Mayo Clinic Imaging Biomarker Discovery Program.References
- Bammer R, Keeling SL, Augustin M, et al. Improved diffusion‐weighted single‐shot echo‐planar imaging (EPI) in stroke using sensitivity encoding (SENSE). Magnetic Resonance in Medicine 2001; 46(3): 548-54.
- Saritas EU, Cunningham CH, Lee JH, Han ET, Nishimura DG. DWI of the spinal cord with reduced FOV single‐shot EPI. Magnetic Resonance in Medicine 2008; 60(2): 468-73.
- Chen N-K, Guidon A, Chang H-C, Song AW. A robust multi-shot scan strategy for high-resolution diffusion weighted MRI enabled by multiplexed sensitivity-encoding (MUSE). Neuroimage 2013; 72: 41-7.
- Holdsworth SJ, Skare S, Newbould RD, Guzmann R, Blevins NH, Bammer R. Readout-segmented EPI for rapid high resolution diffusion imaging at 3T. European journal of radiology 2008; 65(1): 36-46.
- In MH, Posnansky O, Speck O. High-resolution distortion-free diffusion imaging using hybrid spin-warp and echo-planar PSF-encoding approach. NeuroImage 2017; 148: 20-30.
- In MH, Tan ET, Trzasko JD, et al. Distortion‐free imaging: A double encoding method (DIADEM) combined with multiband imaging for rapid distortion‐free high‐resolution diffusion imaging on a compact 3T with high‐performance gradients. J Magn Reson Imaging 2020; 51(1): 296-310.
- Setsompop K, Gagoski BA, Polimeni JR, Witzel T, Wedeen VJ, Wald LL. Blipped‐controlled aliasing in parallel imaging for simultaneous multislice echo planar imaging with reduced g‐factor penalty. Magnetic resonance in medicine 2012; 67(5): 1210-24.
Figures
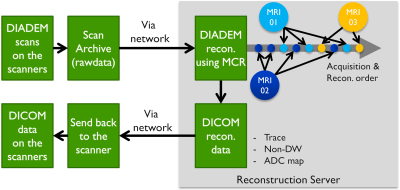
Figure 1. Flowchart of online
DIADEM reconstruction pipeline
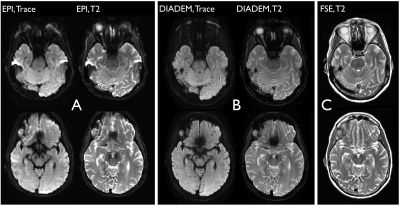
Figure 2. Comparison of EPI- (A) and DIADEM-based
DWI (B) images obtained on a small-bore whole-body 3T scanner (MR750). T2 FSE
reference images are provided for comparison (C). Two slices were chosen to
demonstrate the effects of local distortions in temporal (upper row) and
frontal lobes (bottom row). In (A) and (B), trace (left column) and T2 (right
column) are shown. The
image resolution for EPI, DIADEM, and FSE are 1.72×0.86×4, 1×1.83×4, and
0.86×0.86×4 mm3, respectively.
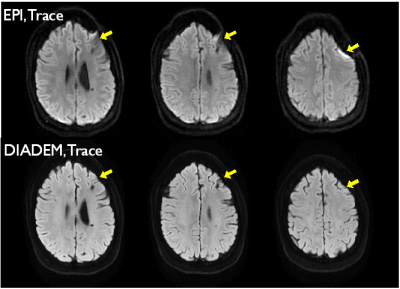
Figure 3. Comparison of metal-induced distortions due to metallic shunt components in EPI-
(upper row) and DIADEM-DWI (bottom row) on a small-bore whole-body 3T scanner (MR750).
Three slices (from left to right column) were chosen to demonstrate the effects
induced by metal-induced susceptibility effects. Yellow arrows indicate the
locations with metal-induced susceptibility effects. Two focal areas of
susceptibility change are more conspicuous on the DIADEM images, and not
mitigated by the distortion correction algorithm.
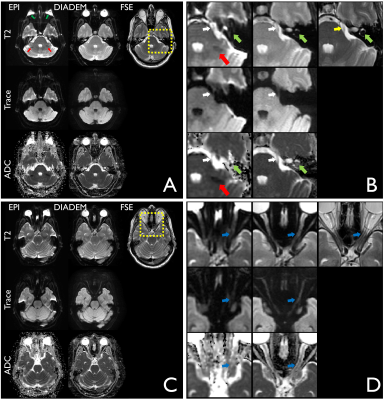
Figure 4.
Comparison of local brain structures in high susceptibility areas in EPI- and
DIADEM-DWI on a small-bore whole-body 3T scanner (MR750). The full FOV (A,C)
and zoomed images (B,D) are shown to
demonstrate the local structures more clearly. In (A,B), dark green-, red-, yellow-, white, and light green-colored
arrows indicate distorted eyeballs, ocular globe Nyquist ghosting artifacts, cisternal
segment of the trigeminal nerve, and
internal auditory canal, respectively. In (C,D), blue arrows indicate
the optic nerve.
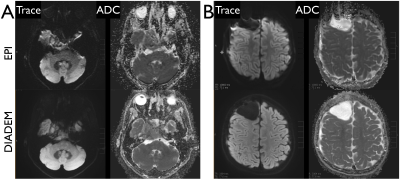
Figure 5.
Comparison of EPI- and DIADEM-DWI in patients with brain tumors (A) and brain
resection (B) on a wide-bore whole-body 3T scanner (MR750W). Less anatomic distortion of the tumor (A) and less susceptibility artifact at the resection bed (B) are clearly shown in DIADEM. The image resolution for EPI and DIADEM are 1.72×0.86×4 and 1.1×1.1×4 mm3,
respectively.
DOI: https://doi.org/10.58530/2022/3289