3247
Multiparametric MRI method development for clinical prostate imaging using 5T MR imaging1Shanghai Institute of Medical Imaging, Shanghai, China, 2United Imaging Healthcare, Shanghai, China, 3Department of Radiology, Zhongshan Hospital, Fudan University, Shanghai, China
Synopsis
Moving to higher magnetic field strength (> 3 T) may have clinical advantages because of an intrinsic increase of the signal-to-noise ratio (SNR), while heterogeneity in the transmit radiofrequency (RF) field or B1 can cause signal voids throughout images. This study aimed to evaluate the development of prostate MRI at 5T by providing assessment of image quality on clinical sequences, including T1W, T2W and DWI images. According to current results about image quality, present of artifacts, visibility of anatomical structures of T2W images, and geometric distortion of DWI images, clinical prostate imaging is feasible at 5T MRI.
Introduction
In recent years, the development of ultra-high-field MR scanners has grown rapidly. A previous study showed that T2-weighted (T2W) imaging with satisfactory to good quality at 7T can be routinely acquired, and cancer lesions were visible in patients with prostate cancer [1]. Moving to higher magnetic field strength (> 3 T) may have clinical advantages because of an intrinsic increase of the signal-to-noise ratio (SNR), which theoretically could be used to increase spatial resolution or reduce imaging time [2]. However, heterogeneity in the transmit radiofrequency (RF) field or B1 can cause signal voids throughout images. Besides, shorter T2-relaxation times and increased sensitivity to susceptibility artifacts can also impair the image quality at 7T MRI [3]. The purpose of this study was to evaluate the development of prostate MRI at 5T by providing assessment of image quality on clinical sequences, including T1-weighted (T1W), T2W and Diffusion-weighted imaging (DWI).Materials and Methods
Ten healthy subjects (mean age, 45.5 ± 7.5) were measured on a 5T MR scanner (uMR Jupiter, United Imaging Healthcare, Shanghai, China), using a 24-channel transmit/receive body array coil. SAR-monitoring and B0 and B1+ shimming were performed. Imaging sequences including: (1) axial T1W quick3d gradient echo (GRE) sequence (TR/TE = 3.34/1.42 ms, FA = 15°, Bandwidth = 850 Hz, 60 slices, Slice thickness = 3 mm, FOV = 300 × 400 mm, Matrix = 410 × 608, Number of averages = 2, Acquisition time = 16.9s); (2) axial T2W fat-saturated fast spin echo (FSE) sequence (TR/TE = 2600/128.24 ms, FA = 90°, Bandwidth = 200 Hz, 30 slices, Slice thickness = 5mm, FOV = 380 × 300 mm, Matrix = 639 × 504 , Number of averages = 2, Acquisition time = 2min10s); and (3) echo-planar imaging (EPI) - DWI (TR/TE = 3650/53 ms, FA = 90°, Bandwidth = 2100 Hz, 30 slices, Slice thickness = 5 mm, FOV = 180 × 380 mm, Matrix = 410 × 608, b = 50, 800 s/mm2, Number of averages = 2, 4).Image analysis was performed by two experienced radiologists in consensus. For all the sequences, overall image quality (5 = excellent; 4 = good; 3 = moderate; 2 = poor; 1 = non-diagnostic) and presence of artifacts (5 = pronounced; 4 = considerable; 3 = moderate; 2 = minimal; 1 = none) were assessed on a 5-point scale. Visibility of anatomical structures, defined as distinction between peripheral and transition zone, seminal vesicles, and delineation of the prostate, was graded on T2W images utilizing a five-point scale (5 = excellent, 4 = good, 3 = satisfactory, 2 = poor, 1 = unacceptable). For DWI images, geometric distortion (defined as modification in size, profile, and/or orientation due to inhomogeneities of the magnetic field in relation to T2W images) was evaluated on a 5-point scale (5 = very high distortion; 4 = high distortion; 3 = intermediate distortion; 2 = low distortion; 1 = no distortion). Mean values and standard deviations (SD) were calculated for all the measured scores. Results are presented as mean ± SD.
Results
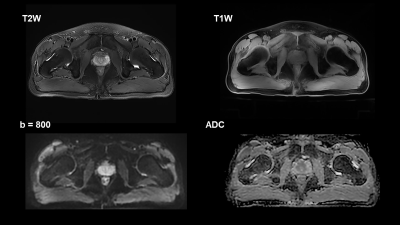
Representative images of two subjects are shown in Figure 1 and 2. Overall image quality was scored as moderate to good in T1W images (3.9 ± 0.5), good to excellent in T2W images (4.1 ± 0.8), and moderate in DWI images (3.0 ± 0.6). Presence of artifacts of T1W, T2W and DWI images were scored as none to minimal (1.5 ± 0.5 for T1W, 1.4 ± 0.5 for T2W, and 1.8 ± 0.5 for DWI).Besides, visibility of anatomical structures for T2W at 5T was graded as good to excellent (4.2 ± 0.7). Upon DWI images at 5T, the geometric distortion was graded as no distortion to low distortion (1.5 ± 0.9).
Discussion & Conclusion
According to the Prostate Imaging Reporting and Data System (PI-RADS), prostate anatomy is mainly visualized by T2-weighted (T2W) imaging [4], while diffusion-weighted imaging (DWI) has been shown to diagnostically outperform all other MRI parameters for lesions located in the peripheral zone (PZ) [5]. Further, T1W imaging is a key component of multiparametric MRI for assessment of post-biopsy hemorrhage [6]. This study proved that multiparametric MRI method, including T1W, T2W and DWI images at 5T can achieve diagnostic image quality. Further study is guaranteed to examine the feasibility of dynamic contrast-enhanced MRI in prostate at 5T.Acknowledgements
No acknowledgement found.References
1. Vos, E., et al., Image quality and cancer visibility of T2-weighted magnetic resonance imaging of the prostate at 7 Tesla. European radiology, 2014. 24(8): p. 1950-1958.
2. Takahashi, M., H. Uematsu, and H. Hatabu, MR imaging at high magnetic fields. European journal of radiology, 2003. 46(1): p. 45-52.
3. Metzger, G.J., et al., Local B1+ shimming for prostate imaging with transceiver arrays at 7T based on subject‐dependent transmit phase measurements. Magnetic Resonance in Medicine: An Official Journal of the International Society for Magnetic Resonance in Medicine, 2008. 59(2): p. 396-409.
4. Weinreb, J.C., et al., PI-RADS prostate imaging–reporting and data system: 2015, version 2. European urology, 2016. 69(1): p. 16-40.
5. Langer, D.L., et al., Prostate cancer detection with multi‐parametric MRI: Logistic regression analysis of quantitative T2, diffusion‐weighted imaging, and dynamic contrast‐enhanced MRI. Journal of Magnetic Resonance Imaging: An Official Journal of the International Society for Magnetic Resonance in Medicine, 2009. 30(2): p. 327-334.
6. Gupta, R.T., et al., PI‐RADS: Past, present, and future. Journal of Magnetic Resonance Imaging, 2020. 52(1): p. 33-53.