3239
High Accuracy Heartbeat Detection with 433MHz CW-Doppler Radar for MRI Application1Department of Electronic Engineering, Tsinghua University, Beijing, China, 2Department of Electrical Engineering, Stanford University, Stanford, CA, United States
Synopsis
This work assesses heartbeat detection by continuous-wave (CW) Doppler radar using low and high carrier frequencies of 433MHz and 5GHz as options for non-contact vitals sensing in MRI. The experimental results show that using the amplitude of received complex signals in low frequency 433MHz-detection can perform as well as 5GHz-detection due to near field interactions within a 20cm range, with similar heartbeat detection efficacy.
INTRODUCTION
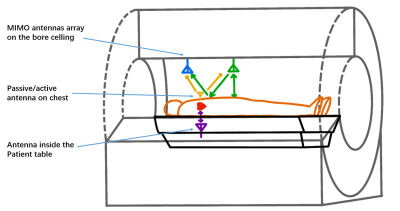
This work assesses heartbeat detection by continuous-wave (CW) Doppler radar at a low carrier frequency of 433MHz for future use in MRI (Figure 1). In conventional MRI, respiratory bellows gating and cardiac gating by ECG or photoplethysmography (PPG) are commonplace to sort MRI data into cardiac phases, but often complicate setup for the patient1. In noncontact vital signs sensing, continuous-wave Doppler radar is widely used at 2.4GHz, 5GHz or even higher. In principle, higher carrier frequencies provide greater phase sensitivity to motion at a distance, but this is only true for equal carrier phase noise2. In MRI, cardiac signal detection will be performed over distances under 20cm, where near field proximity and low frequency field penetration can modulate the reflected signal. Here, a software-defined radio (Nuand bladeRF 2.0 SDR) is configured to assess in-vivo heart beat detection under free-breathing conditions for 20cm range at a low 433MHz and typical 5GHz carrier. The radar system adopts a single channel heterodyne receiver architecture using the bladeRF and dual antennas. The radar cardiac signals were validated with a reference PPG signal.METHODS
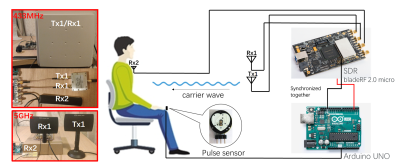
The experimental setup is shown in Figure 2. The radar system exploits one transmit channel and two receive channels, with Tx1 and Rx1 antennas 20cm away from the chest, and an Rx2 antenna on the subject's chest. Rx2 maximizes near field sensitivity for potential bistatic radar configurations, if feasible. For 433MHz detection, the Tx1 and Rx1 channel shared one antenna via a power splitter (Figure 2). For 5GHz detection, the Tx1 and Rx1 channels used separate antennas. The PPG sensor (PulseSensor.com) was interfaced to an Arduino UNO, and synchronized with the SDR to sense the index finger pulse. The sampling rates of the SDR and PulseSensor were 1MHz and 500Hz, respectively. The radar and PPG signals were down-sampled to 100Hz by MATLAB post-processing, using a lowpass Chebyshev Type I IIR filter of order 8. Vital sign measurements were repeated 10 times - each trial containing a 10-second time series. The signals were then bandpass filtered to select the cardiac band (0.6Hz to 2Hz) using cascaded IIR lowpass and highpass filters in MATLAB. Finally, Singular Spectrum Analysis (SSA) was applied to decompose the time-domain signals into different reconstruction components. The reconstruction components were selected based on prior knowledge of the heartbeat waveform3. Ultimately, the radar cardiac pulse “trigger” was extracted and compared with the reference PPG signal. To evaluate the accuracy of the reconstruction, the average time error between the radar and PPG pulses were calculated after removing the influence of Pulse Transit Time (PTT).For the free-breathing 5GHz radar signals, a compensation of DC offset based on L2-norm minimization was also applied when processing the radar signals4.
RESULTS
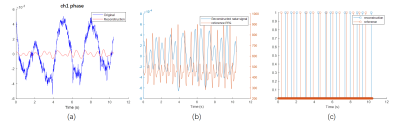
Figure 3 shows a reconstruction using the phase of the complex radar signal from receiving channel 1 after down conversion with the 433MHz detection under free-breathing condition. In 3(a), the original filtered radar signal (blue) and recovered heartbeat waveform after SSA (red) are shown. Figure 3(b) shows the recovered heartbeat waveform (blue), and the reference PPG signal (orange). In 3(c), two sequences of pulses extracted from the recovered heartbeat waveform and the reference PPG signal are compared to evaluate the reconstruction quality. Unpaired pulses at the beginning or end of the sequences, caused by PTT, were removed when evaluating the reconstruction. Figure 4 displays histograms of unmatched pulse numbers between reconstruction and reference using different post-processing. Figure 5 shows the average time error between the reconstruction and reference pulses after removing unmatched pulses. When calculating the average time error of reconstruction, the constant time shift in each pulse pair, caused by PPT and estimated by the average time shift in pairs, was subtracted from the original time shifts in each pair, and the absolute values of the residues were summed up and averaged into the time error. From Figure 4 and 5, with 433MHz-detection, the reconstruction of heartbeats using the amplitude of complex signal is better than that from phase-only in both free-breathing and breath-hold cases. Use of the amplitude of complex signal at 433MHz also outperformed the traditional method of using phase at 5GHz to reconstruct the heartbeat under free-breathing conditions.DISCUSSION
433MHz-detection has about 10x larger wavelength than 5GHz-detection, which ought to reduce phase sensitivity to motion accordingly. However, for short-range detection of 20cm, near-field effects at 433MHz cause significant amplitude and phase modulation from cardiac activity in the complex radar signal. This phenomenon is enhanced even more by a one-way (bistatic) radar signal instead of the reflected signal. This should be expected since the 433 MHz ISM band corresponds to a 10T MRI frequency. Interestingly, while CW Doppler traditionally relies on phase-based group delay, once the full complex signal is processed, the outcome is entirely equivalent to impedance sensing.CONCLUSION
This work demonstrates the possibility of heartbeat detection using CW Doppler radar in the 433MHz ISM band. A new evaluation criterion for reconstruction by calculating the average time error is proposed in the work, which aims to generate retrospective radar-based cardiac gating for MRI. Experimental results show that the low frequency 433MHz-detection can perform as well as 5GHz-detection.Acknowledgements
NIH grants: U01EB029427, R01EB01924105, R01EB012031, U01EB026412, GE HealthcareReferences
[1] Rosenzweig, S. , et al. "Cardiac and Respiratory Self-Gating in Radial MRI using an Adapted Singular Spectrum Analysis (SSA-FARY)." IEEE Transactions on Medical Imaging PP.99(2020):1-1.
[2] Li, C. , et al. "A Review on Recent Advances in Doppler Radar Sensors for Noncontact Healthcare Monitoring." IEEE Transactions on Microwave Theory and Techniques 61.5(2013):2046-2060.
[3] Ghaderi, F. , H. R. Mohseni , and S. Sanei . "Localizing Heart Sounds in Respiratory Signals Using Singular Spectrum Analysis." Biomedical Engineering IEEE Transactions on 58.12(2011):p.3360-3367.
[4] Zakrzewski, M. , H. Raittinen , and J. Vanhala . "Comparison of Center Estimation Algorithms for Heart and Respiration Monitoring With Microwave Doppler Radar." IEEE Sensors Journal 12.3(2012):627-634.
Figures