3170
Preoperative Prediction of Lymph Node Metastasis in Patients With Rectal Cancer Using A Multi-Modality Radiomics Model
Rui Wu1, Weiqiang Dou2, and Aiyin Li3
1Department of radiology, Shandong Provincial Qianfoshan Hospital, Cheeloo college of Medicine, Shandong University, Jinan, China, 2MR Research, GE Healthcare, Beijing, China, 3Department of radiology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan, China
1Department of radiology, Shandong Provincial Qianfoshan Hospital, Cheeloo college of Medicine, Shandong University, Jinan, China, 2MR Research, GE Healthcare, Beijing, China, 3Department of radiology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan, China
Synopsis
This study mainly aimed to build a multi-modality radiomics model for predicting lymph node metastasis (LNM) of rectal cancer (RC) preoperatively. 82 RC patients were enrolled in this study. Two, six, four and eleven optimal features were separately selected for venous phase CT, HR-T2WI, DWI and multi-modality by incorporating CT, HR-T2WI and DWI together. Together with MRI-reported LN status feature, clinical features, and the combination of multi-modality and clinical features, in total seven support vector machine (SVM) classification models were respectively built. Incorporated with clinical features, multi-modality radiomics model provided the most robust predictive performance in predicting LNM.
Introduction
Nowadays, colorectal cancer (CRC) is the second leading overall cause of cancer death as well as the fourth cause of cancer mortality for human beings worldwidely.1,2 Lymph node metastasis (LNM) has been reported previously the most important prognostic indicator for patients with rectal cancer (RC).3 Therefore, accurate assessment of LN status before surgery is crucial for RC patients in tumor staging, treatment, prognosis and survival.Computed tomography (CT) and T2-weighted imaging (T2WI) features of the primary tumor were previously applied in radiomics models to well predict LNM in colorectal and rectal cancer patients.4,5 Based on these findings, we assumed that it might hold clinical potential to apply multiparametric magnetic resonance imaging (MRI), together with CT, in predicting LN status for RC patients.
Therefore, this study aimed to investigate the clinical feasibility of a multi-modality radiomics model by incorporating venous phase CT and MRI (i.e., high resolution T2-weighted imaging (HR-T2WI) and diffusion weighted imaging (DWI)) features as well as clinical features in predicting LNM of rectal cancer preoperatively.
Materials and Methods
SubjectsThis study retrospectively collected 82 RC patients (57 males and 25 females,mean age:63.1210.859 years old ) confirmed by histopathological examination. Each patient had pelvic contrast-enhanced CT and MRI examination within 2 weeks before surgery, and subsequent radical surgical resection was performed. LN dissections were performed, and all LNs were assessed by pathological examination. Baseline clinicopathologic data, including age, gender, laboratory measurements before surgery (i.e., CEA, CA199, CA724), tumor size and T stage, were collected.
Imaging acquisition
For each patient, standard dynamic contrast-enhanced CT scan (Discovery HD750; GE Healthcare) was implemented with the following scan parameters of tube voltage 120kV, tube current 100-420mA, rotation time of 0.7s, slice thickness of 5mm, pitch of 0.984, field of view (FOV) of 425mm×425mm and matrix size of 512×512.
Additionally, pelvic MRI was also performed using 3.0T MRI (Discovery 750; GE Healthcare) with an 8-channel phased array coil, including sagittal T2WI, axial oblique HR-T2WI, and DWI. For DWI, b values of 0 and 1000 s/mm2 were applied. The detailed parameters for each sequence are presented in Table 1.
Data analysis
All statistic analyses were performed with SPSS software. Univariate and multivariate logistic regression analysis were used to identify the clinical risk factors significantly associated with pathological LNM. A value of P < 0.05 was considered the threshold of statistical significance.
Feature standardization, selection and model building were performed using Python 3.6. The regions of interest (ROI) were manually segmented along the tumor border over multi-slice of venous phase CT, HR-T2WI, and DWI at b-value of 1000s/mm2 (Figure 1). 1409 radiomics features were extracted in three categories from each imaging modality. Inter- and intra-class correlation coefficients (ICCs) were computed for evaluating the robustness of all features. Features with both inter- and intra-observer ICCs ≥0.75 were applied for subsequent analysis. The variance threshold, Select_K_Best, and the least absolute shrinkage and selection operator (LASSO) methods were then applied for feature selection.
Seven support vector machine (SVM) classification models were, respectively, built based on features of venous phase CT (ModelCT), of HR-T2WI (ModelT2WI), of DWI (ModelDWI), of combined three imaging (ModelMM), of MR-reported LN status (ModelMRI-reported LN ), of clinical risk factors (Modelclinical), and of the combination of multiple imaging modality and clinical risk factors (Modelcombined). Each model performance in predicting LNM was separately assessed by receiver operating characteristic (ROC) derived area under curve (AUC) analysis.
Results
Using multivariate logistic regression analysis, proportion of the tumor occupied lumen circumferential (tumor_circumference_length) was identified as a clinical risk factor of rectal cancer patients with LNM (Table 2). In addition, T stage and MRI-reported LN status were also included as clinical risk factors. The clinical model was developed based on these three clinical risk factors. In total, 4227 radiomics features were extracted from CT, HR-T2WI and DWIb1000. After the Select_K_Best and LASSO logistic regression algorithm methods were applied with the variance threshold, two, six, four, and eleven remaining features were selected for each image type respectively (Figure 2a, b, c, d). Using ROC analysis, the corresponding AUC values of all seven models were shown in Figure 3. ModelMM, combining all three types of imaging data, showed better predictive efficacy with higher AUC of 0.782 than ModelCT (0.737), ModelT2WI (0.615) or ModelDWI (0.583), and comparable prediction with Modelclinical with AUC of 0.792. Together with clinical risk factors, Modelcombined showed the highest discrimination ability for predicting LNM with AUC of 0.840.Discussion and Conclusions
This study mainly developed a multi-modality radiomics model in predicting LNM for patients with rectal cancer before surgery. The radiomics model including multi-modality features of venous CT, HR-T2WI and DWI showed more robust performance in LNM prediction than each imaging type alone. Considering a high impact on guiding preoperative treatment, T stage, MRI-reported LN status as well as a clinical feature in radiomics analysis were considered to form a clinical model. Incorporating these three clinical risk factors, the combined multi-modality model provided the highest discrimination ability in predicting LNM.In conclusion, the multi-modality radiomics model, including CT, HR-T2WI and DWI features, has been developed and validated in predicting LNM for RC patients preoperatively.Acknowledgements
No.References
1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019; 69:7-34.2.Mattiuzzi C, Lippi G. Current Cancer Epidemiology. J Epidemiol Glob Health. 2019; 9:217-222.
3.Kwon TS, Choi SB, Lee YS, Kim JG, Oh ST, Lee IK. Novel Methods of Lymph Node Evaluation for Predicting the Prognosis of Colorectal Cancer Patients with Inadequate Lymph Node Harvest. Cancer Res Treat. 2016; 48:216-224.
4.Huang YQ, Liang CH, He L, et al. Development and Validation of a Radiomics Nomogram for Preoperative Prediction of Lymph Node Metastasis in Colorectal Cancer. J Clin Oncol. 2016; 34:2157-2164.
5.Li J, Zhou Y, Wang X, Zhou M, Chen X, Luan K. An MRI-based multi-objective radiomics model predicts lymph node status in patients with rectal cancer. Abdom Radiol (NY). 2021; 46:1816-1824.
Figures
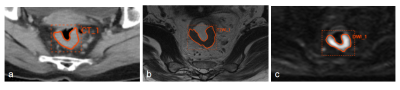
Figure 1 | Example images for rectal cancer contouring in a 60 years old patient. The outline of regions of interest on one slice of axial venous phase CT image (a), high resolution T2-weighted MR image (b) and DWI at b-value of 1000s/mm2 (c).
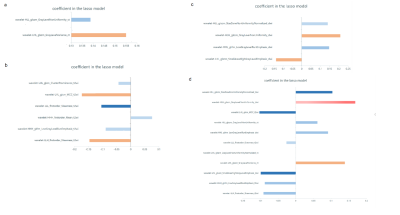
Figure 2 | Radiomics features selected by least absolute shrinkage and selection operator (LASSO) algorithm. X-axis means the coefficient in Lasso Model. Y-axis means the optimal features selected from different feature subsets. Two, six, four and eleven optimal features were selected from CT ( a ),T2WI ( b ),DWI ( c ) and combined three imaging modalities features ( d ) , respectively.
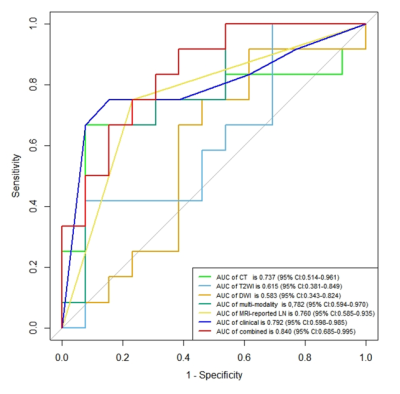
Figure 3 | Receiver operating characteristic (ROC) curves of the radiomics features derived from CT, T2WI, DWI, multi-modality imaging, MRI-reported LN status, clinical risk factors and the combination of multi-modality imaging with clinical risk factors in the testing cohort.
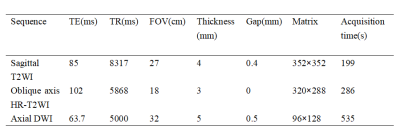
Table 1 Detailed scan parameters of each MR sequence
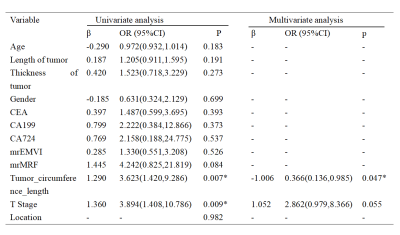
Table 2 Univariate and multivariate analysis to determine the final clinical risk factors of lymph node metastasis
DOI: https://doi.org/10.58530/2022/3170