3141
The relationship between pubic bone and pubococcygeus muscle injury in transvaginal delivery primiparas using MRI1Department of Radiology, Tianjin First Central Hospital, Tianjin, China, 2Philips healthcare, Beijing, China
Synopsis
As transvaginal delivery may led to bony and soft birth canal injury, this study aimed to explore the possible relationship between the pelvic bones injury and the pelvic floor support muscles injury. In this study, we found that the pubic injury with significant clinical symptom may suggest the occurrence of pubococcygeus muscle injury with hidden symptoms. With the increased severity of the pubic bone injury, the higher the rate and severity of pubococcygeus muscle injury could be detected, which could be used to guide the clinical evaluation of abnormalities and corresponding rehabilitation treatment in time.
Purpose
In this study, we aim to 1) explore the correlation between the occurrence of pubic injury and pubococcygeus muscle injury; 2) assess the relationship between the occurrence and its severity in primiparas during vaginal delivery.Method
Pelvic MR images of 88 cases of primiparous women who underwent transvaginal delivery at 42 days postpartum were retrospectively analysis in our hospital from October 2016 to December 2017. The inclusion criteria included: 1. primiparas who delivered vaginally; 2. 37 weeks+ of gestation, single birth; 3. primiparas who understand the purpose and process of the experiment, and agree to be a subject to obtain clear images. The exclusion criteria included: 1. primiparas with a history of pelvic diseases or trauma; 2. primiparas with a history of pelvic surgery. 3. primiparas without clear images and complete clinical information. According to the MRI images, the parturient were separated to pubic injury group and non-pubic injury group.The MR examination was performed using a 3T MR scanner (Philips, Ingenia, Netherlands). Primiparas were examined in the supine position with a 16-channel body matrix array coil. The MRI sequences included fast spin echo (FSE) T2 weighted and fat suppression T2 weighted sequences (TR=4110ms; TE=102ms; matrix=320 x 256; FOV=260mm×260mm; section thickness=3mm; voxel=0.6mm x 0.5mm x 3.0mm; averages 2 times). The scanning range extended from the upper edge of the femoral heads on both sides, down to the lower edge of the perineal body, with bilateral ischial spines on both sides. The images on sagittal, coronal, and transverse planes were reconstructed and acquired. The injury status (including no injury, pubic bone marrow edema, pubic fractures, and pubococcygeus muscle edema, tear and rupture) of the pubis and pubococcygeus muscle were evaluated by two senior radiologists, and were scored for disease severity. Chi-square test was used to explore the group differences in the proportion of pubococcygeus muscle injury. The correlation between the score of pubic injury and the score of pubococcygeus muscle injury was tested by Kendall`s tau-b correlation analysis.
Result
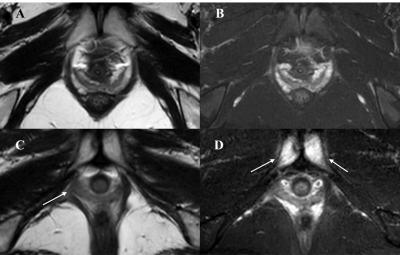
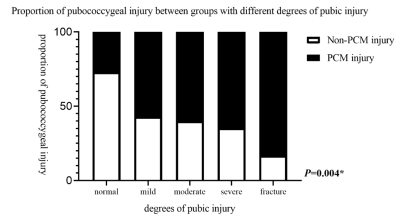
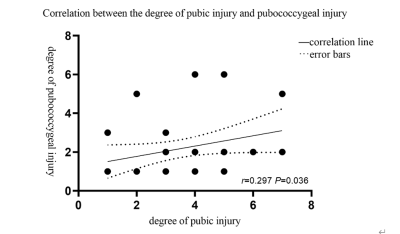
There is a significant difference in the incidence of pubococcygeus muscle injury between the pubic injury group and the non-pubic injury group (67% vs 27%, P = 0.000). The detailed results are shown in figure 1. Figure 2 show the image examples from two patients. The incidence of pubococcygeus muscle injury varies according to the score of pubic bone injury (P = 0.004). Figure 3 shows the proportion of pubococcygeal muscle injury between groups with different degrees of pubic bone injury. The women with pubic fractures have higher rates of pubococcygeus muscle injury. In addition, there is a positive linear relationship between the degree of pubic bone injury and the degree of pubococcygeus muscle injury (P = 0.036, see Figure 4).Conclusion
In this study, we found that the vaginal delivery primipara with pubic bone injury is associated with the pubococcygeus muscle injury. With the increased severity of the pubic bone injury, there is the higher the rate and severity of pubococcygeus muscle injury. Meanwhile, there is a positive correlation between the severity of pubic bone injury and the severity of pubococcygeus injury. The data suggested that the possibility of pelvic floor supports soft tissue structures injuries should also be considered, when women undergoing vaginal delivery have clinical symptoms such as pain in the pubic area, in addition to the vigilance of pelvic bones injury.Acknowledgements
We sincerely thank the participants in this study.References
[1] Turner C E , Young J M , Solomon M J , et al. Incidence and Etiology of Pelvic Floor Dysfunction and Mode of Delivery: An Overview[J]. Diseases of the Colon & Rectum, 2009, 52(6):1186-95.
[2]Brandon C , Jacobson J A , Low L K , et al. Pubic bone injuries in primiparous women: magnetic resonance imaging in detection and differential diagnosis of structural injury[J]. Ultrasound in Obstetrics & Gynecology, 2012, 39.
[3] Miller J M , Low L K , Zielinski R , et al. Evaluating maternal recovery from labor and delivery: bone and levator ani injuries[J]. American Journal of Obstetrics & Gynecology, 2015, 213(2):188.e1-188.e11.
[4] Nattiv A , Kennedy G , Barrack M T , et al. Correlation of MRI grading of bone stress injuries with clinical risk factors and return to play: a 5-year prospective study in collegiate track and field athletes.[J]. American Journal of Sports Medicine, 2013, 41(8):1930-1941. DOI: 10.1177/0363546513490645
[5] Mueller-Wohlfahrt HW, Haensel L, Mithoefer K, et al. Terminology and classification of muscle injuries in sport: the Munich consensus statement.[J]. Br J Sports Med 2013;47:342-50.
[6] Shi M , Shang S , Xie B , et al. MRI changes of pelvic floor and pubic bone observed in primiparous women after childbirth by normal vaginal delivery[J]. Archives of Gynecology & Obstetrics, 2016, 294(2):285-289.
[7] Erica Eason, Michel Labrecque, Sylvie Marcoux, et al. Effects of carrying a pregnancy and of method of delivery on urinary incontinence: a prospective cohort study[J]. BMC Pregnancy and Childbirth, 2004.
[8] Lien K C , Mooney B , Delancey J O L , et al. Levator Ani Muscle Stretch Induced by Simulated Vaginal Birth[J]. Obstetrics & Gynecology, 2004, 103.
[9] Kearney R , Sawhney R , Delancey J O L . Levator Ani Muscle Anatomy Evaluated by Origin-Insertion Pairs[J]. Obstetrics & Gynecology, 2004, 104(1):168-173.
[10] Miller J M , Brandon C , Jacobson J A , et al. MRI findings in patients considered high risk for pelvic floor injury studied serially after vaginal childbirth.[J]. Ajr American Journal of Roentgenology, 2010, 195(3):786-91.
[11] Agten C A , Metzler C , Rosskopf A B , et al. MR imaging of pubic symphysis after uncomplicated vaginal delivery and planned caesarean delivery in the first postpartum week[J]. Clinical Imaging, 2019, 56:58-62.
Figures