3118
Applicable diagnostic model for detecting patients with mental disorders with magnetic resonance imaging1Department of Radiology, West China Hospital of Sichuan University, Chengdu, China, 2Department of Research and Development, Shanghai United Imaging Intelligence Co., Ltd., Shanghai, China
Synopsis
To yield clinical utility in mental disorder identification individually, we used a multiple instance learning-based method to construct a digital model based on clinical MRI scans for automated detection of patients with psychiatric disorders. An accuracy of 84% was achieved in the primary dataset with 19453 subjects, and 76% in external dataset with 600 subjects. A higher sensitivity was achieved in identifying high-risk subjects than self-scaled questionnaires (71.1% vs 22.2%) in 148 prospectively recruited college students. With a complete workflow of development and validation, the constructed model is more practical to be translated in high-risk subject screening among vulnerable populations.
INTRODUCTION
Pattern recognition methods applied to neuroimaging data in mental disorders could yield future clinical utility in disorder identification and differential diagnosis individually. However, previous constructed models for specific disorder diagnosis barely considered the clinical context to be applied and potentially against health economics, none thereof has been translated into clinical practice. The present study aims to develop a more practical model for mental problem screening among vulnerable populations.METHODS
The clinical MRI scans including T1- and T2-weighted imaging of 14915 patients with different psychiatric disorders and 4538 healthy controls were retrospectively recruited. A multiple instance learning-based (MIL) method 1 was adopted to train and test a computer-assisted diagnosis (CAD) model. All the patients were combined as a whole during the model construction, and data of 80% of the participants were included in the training dataset while the rest was used for testing. An independent dataset with 600 subjects were used to test the generalization of the model. Finally, to show brain regions that contributed greatly to the psychiatric patient identification during the deep learning, we employed the class activate map (CAM) to visualize the decision process of MIL network. We also tailored an anisotropic 3D Resnet-60 as the comparison model for CAD of mental disorders in end to end. This model is derived from Residual neural network (ResNet), which has the best classification effect in 2D natural images 2. The data and environment of experiments with Resnet-60 for training and testing were conformed to MIL. To examine the real-world utility, we prospectively collected 148 subjects who had generally high prevalence for mental disorders, and evaluated the efficacy of the CAD model in identifying psychologically high-risk subjects and compared it to self-ratings with questionnaires against the psychiatric interviewing.RESULTS
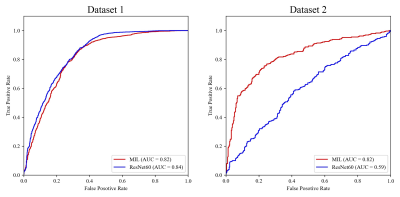
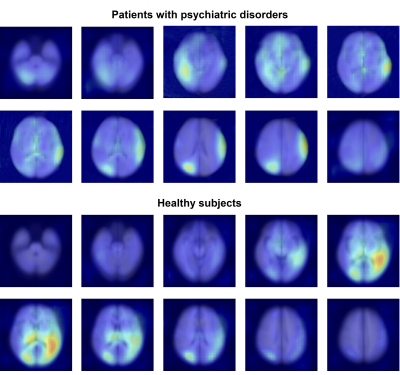
In the primary dataset, the MIL network successful differentiated patients with psychiatric disorders from healthy controls with an accuracy of 0.84 (sensitivity=0.94, specificity=0.52, AUC=0.82). By contrast, the ResNet-60 model achieved an accuracy of 0.81 in patient/control classification (sensitivity=0.86, specificity=0.68, AUC=0.84). In the validation dataset, with the established MIL model, the patients could be successfully differentiated from healthy controls with an accuracy of 0.76 (sensitivity=0.66, specificity=0.85, AUC=0.82), whereas the ResNet-60 model achieved an accuracy of 0.53 (sensitivity=0.77, specificity=0.29, AUC=0.59), with inferior performance of generalization to MIL. The ROC curves of the classification performance of MIL network and ResNet-60 in primary and validation datasets were presented in Figure 1. The generated CAM map exhibited regions to which MIL network paid more attention when making a diagnosis on an object and the regions that contributed greatly to the patient identification were mainly cortical, and located in right precuneus, left superior temporal gyrus, right inferior temporal gyrus, left precentral/postcentral gyrus, bilateral medial prefrontal cortex and right cerebellum (Figure 2). In the prospective study, a higher sensitivity of this model was achieved in identifying high-risk subjects than the self-ratings with questionnaires (71.1% vs 22.2%), against the gold standard of the in-person interview by an experienced psychiatrist.DISCUSSION
While MRI examinations for patients with mental disorders in clinical practice are commonly used for exclusionary diagnosis to make sure no visible abnormalities such as tumors or encephalitis that potentially cause the psychiatric symptoms, our study creatively developed a specific and precise MIL model with clinical MRI scans to automatically identify patients with psychiatric disorders, of which the stability has also been confirmed in external validation dataset. More importantly, a comprehensive prospective study was further conducted to test the model’s capability in real-world scenario for screening subjects with clinical high risk, and a higher individual sensitivity was achieved than self-ratings with questionnaires, and with less time spent (4 min vs 7 min). For the first time, the clinical-used MRI imaging were found with value in deterministic diagnosis by directly identifying subjects with psychiatric disorders, which had never been achieved before. The regions that contribute to patient identification, including those within default mode network (DMN), somatomotor network (SMN) and cerebellum, have been widely recognized in patients with different psychiatric disorders 3-5. With a complete workflow of development and validation procedures from laboratory to real-world settings for clinical application, our study indicated a digital model that is practical and of great significance as a common clinical examination to identify clinically high-risk individuals for psychiatric disorders in vulnerable populations such as college students and white-collar employees, so as to intervene therapeutically in time to prevent the onset of the illness and improve the outcomes.CONCLUSION
Our study constructs a digital model based on clinical MRI scans for automated detection of patients with mental disorders, with decent accuracy and high sensitivity individually, thus is practical and of great possibility being translated into clinical practice for high-risk subject screening in vulnerable populations.Acknowledgements
This study was supported by the National Natural Science Foundation of China (Project Nos. 8212018014 and 82101998), and Sichuan Science and Technology Program (Project Nos. 2021JDTD0002 and 2020YJ0018).References
1. Dietterich, T.G., R.H. Lathrop, and T. Lozano-Pérez, Solving the multiple instance problem with axis-parallel rectangles. Artificial Intelligence, 1997. 89(1): p. 31-71.
2. Chen, Q., et al., A Deep Learning-Based Model for Classification of Different Subtypes of Subcortical Vascular Cognitive Impairment With FLAIR. Front Neurosci, 2020. 14: p. 557.
3. Whitfield-Gabrieli, S. and J.M. Ford, Default mode network activity and connectivity in psychopathology. Annu Rev Clin Psychol, 2012. 8: p. 49-76.
4. Li, C., et al., Transdiagnostic time-varying dysconnectivity across major psychiatric disorders. Hum Brain Mapp, 2021. 42(4): p. 1182-1196.
5. Zhang, W., et al., Brain structural correlates of familial risk for mental illness: a meta-analysis of voxel-based morphometry studies in relatives of patients with psychotic or mood disorders. Neuropsychopharmacology, 2020. 45(8): p. 1369-1379.
Figures