3109
Preliminary study of various models of DWI and diffusion kurtosis imaging on differential diagnosis of spinal metastase and chordoma1Department of Radiology, Peking Union Medical College Hospital, Beijing, China, 2Peking University Third Hospital, Beijing, China
Synopsis
Metastases and chordoma are both malignant tumors. When the manifestations are not typical, the two are prone to misdiagnosis. DWI using a biexponential model measured ADC, D, D*, and f. DWI using a stretched-exponential model obtained DDC, and α. DKI derived MD and MK. The monoexponential, biexponential, and stretched-exponential models of DWI and DKI have differential diagnostic value for spinal metastases and chordoma. Among the single parameter values, the D value has the highest AUC. Combining the values of three parameters (D, f, and α) can significantly improve the diagnostic efficiency of identifying spinal metastases and chordoma.
Introduction and Purpose
Metastases and chordoma are both malignant tumors 1. Both are also common spinal malignancy, and the conventional imaging manifestations are similar. However, if the manifestations are not typical, especially when the metastasis occurs in the skull base and the sacrococcyx, typical imaging characteristics are often not available, and the two are prone to misdiagnosis. Proper preoperative imaging diagnosis is crucial to the selection of treatment methods and prognosis evaluation. MRI has certain limitations in providing sufficient microstructural information and quantitative assessment of disease progression2 . In recent years, functional MRI technology has been increasingly used to evaluate the nature of various tumors, providing a basis for the differential diagnosis of benign and malignant lesions, tumor grading, and prognosis prediction 3. However, research regarding musculoskeletal lesions remains relatively rare 4,5, and research on spinal metastases and chordoma has not been reported. This study aimed to explore the value of monoexponential, biexponential, and stretched-exponential models of DWI and diffusion kurtosis imaging (DKI) for the differential diagnosis of spinal metastases and chordoma.Methods
This retrospective study was approved by the ethics committee of our hospital, and the requirement for informed consent was waived. Patients who had consented to undergo spinal MRI at our hospital were enrolled from September 2017 to January 2020. The following patients were included: patients who had not undergone surgery, needle biopsy, or chemoradiotherapy before MRI and patients with spinal tumors confirmed by surgery or puncture pathology. The following exclusion criteria were applied: contraindication for MRI examination (n = 1); lesions that were too small to outline the region of interest (ROI; focal diameter < 3 cm) (n = 4); thoracic tumors, due to respiratory motion artifacts or heart and large vessel pulsation artifacts that may affect DKI parameter measurement (n = 4); poor image quality unusable for analysis (n = 2). MRI scans were obtained using the GE Discovery MR750 3.0T MRI scanner (GE Healthcare, Piscataway, NJ, USA) in the supine position. All patients underwent conventional plain scans, multi-b value DWI, and DKI scans. The scan parameters were as follows. DWI using a biexponential model measured isotropic apparent diffusion coeffcient (ADC), true diffusion coefficient (D), pseudodiffusion coefficient (D*), and perfusion fraction (f). DWI using a stretched-exponential model obtained water molecular distributed diffusion coefficient (DDC), and intravoxel water diffusion heterogeneity (α). DKI derived mean diffusivity (MD) and mean kurtosis (MK). Independent sample t-testing compared statistical differences among parameters. Sensitivity, specificity, and area under the receiver operating characteristic (ROC) curve were determined. Pearson correlation analysis evaluated the parameters’ correlations.Results
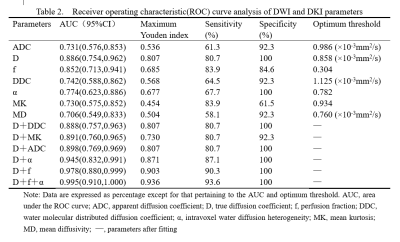
A total of 44 cases were included in the study, including 31 cases of spinal metastases and 13 cases of spinal chordoma. Figures 1 and 2 are pseudo-color diagrams of the parameters for spinal metastases and chordoma. The results were summarized in Tables 1 and 2. ADC, D, f, DDC, α, and MD were significantly lower in spinal metastases than chordomas (all P < 0.05). MK was significantly higher in spinal metastases than chordomas (P < 0.05). D had the highest area under the ROC curve (AUC) of 0.886, greater than MD (AUC = 0.706) or DDC (AUC = 0.742) in differentiating the two tumors (both P < 0.05). Combining D with f and α statistically significantly increased the AUC for diagnosis (to 0.995) relative to D alone (P < 0.05). There was a certain correlation among DDC, ADC and D (all P < 0.05): DDC was positively correlated with ADC and D (r = 0.974 and 0.427, respectively); D and ADC were also weakly positively correlated (r = 0.360).Discussion
In this study, the ADC, D, DDC, α, and MD values of spinal chordoma were significantly higher than those of metastatic tumors, while the MK value was significantly lower than that of metastatic tumors. Possible reasons include metastatic tumors being denser than chordoma—the resulting small cell gaps limit the diffusion of water molecules—and metastatic tumor cells being more heterogeneous due to their quicker proliferation that can easily cause changes such as ischemia and necrosis. This study also conducted correlation analysis among DDC, ADC, and D: DDC was positively correlated with ADC and D; D and ADC were also weakly positively correlated, indicating a certain consistency among the three in reflecting the diffusion movement of water molecules. The D value being lower than the ADC further confirmed that the monoexponential model of DWI contained the microperfusion effect, and did not truly reflect the theory of the limited degree of diffusion of water molecules in tissue. Among the single parameter values, the D value had the highest diagnostic value for differentiating spinal metastases and chordoma, and therefore is potentially clinically applicable. However, a combined diagnosis using D, f, and α had statistically significantly greater AUC (0.995) than the D value alone (Z = 2.185, P < 0.05), indicating that the combined application of IVIM and stretched-exponential model parameters can improve the diagnostic efficiency relative to the single D value.Conclusion
Monoexponential, biexponential, and stretched-exponential models of DWI and DKI can potentially differentiate spinal metastases and chordomas. D combined with f and α performed best.Acknowledgements
We sincerely thank the participants in this study.
References
1. Zambo I, Vesely K. WHO classification of tumours of soft tissue and bone 2013: the main changes compared to the 3rd edition. Cesk Patol. 2014;50:64-70.
2. Wang F, Chu C, Zhao C, et al. Diffusion kurtosis imaging in sacroiliitis to evaluate the activity of ankylosing spondylitis. J Magn Reson Imaging. 2019;49:101-108.
3. Bai Y, Lin Y, Tian J, et al. Grading of Gliomas by Using Monoexponential, Biexponential, and Stretched Exponential Diffusion-weighted MR Imaging and Diffusion Kurtosis MR Imaging. Radiology. 2016;278:496-504.
4. Ogawa M, Kan H, Arai N, et al. Differentiation between malignant and benign musculoskeletal tumors using diffusion kurtosis imaging. Skeletal Radiol. 2019;48:285-292.
5. Wu G, Xie R, Liu X, et al. Intravoxel incoherent motion diffusion MR and diffusion kurtosis imaging for discriminating atypical bone metastasis from benign bone lesion. Br J Radiol. 2019;92: 20190119.
Figures
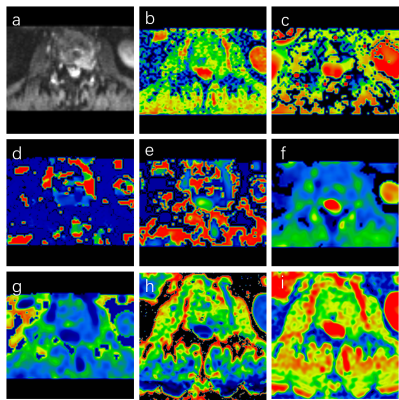
Female, 67 years old, showing metastases of L2 vertebrae from lung cancer. (a) The lesion showed high signal on DWI image; (b) ADC value was 0.970 × 10-3 mm2/s; (c) D value was 0.662 × 10-3 mm2/s; (d) D* value was 4.820 × 10-3 mm2/s; (e) f value was 0.304; (f) DDC value was 1.004 × 10-3 mm2/s; (g) α value was 0.829; (h) MK value was 1.150; (i) MD value was 0.680 × 10-3 mm2/s.
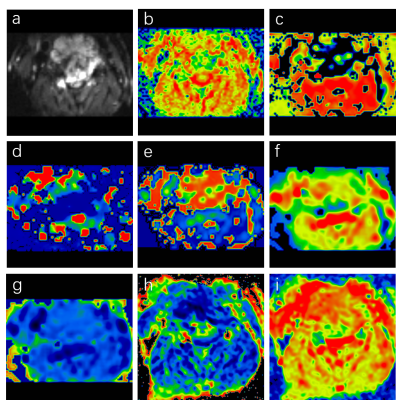
Male, 62 years old, showing chordoma of C4 vertebrae. (a) The lesion showed high signal on DWI image; (b) ADC value was 1.26 × 10-3 mm2/s; (c) D value was 0.884 × 10-3 mm2/s; (d) D* value was 2.550 × 10-3 mm2/s; (e) f value was 0.650; (f) DDC value was 1.385 × 10-3 mm2/s; (g) α value was 0.864; (h) MK value was 0.934; (i) MD value was 0.912 × 10-3 mm2/s.
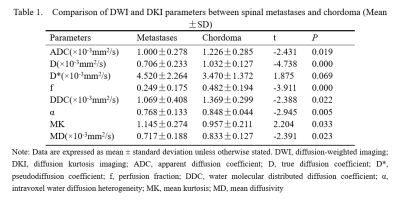
Table 1. Comparison of DWI and DKI parameters between spinal metastases and chordoma.