3069
Effect of 1 Hz rTMS on functional connectivity in Parkinson’s Disease.
Priyanka Bhat1, S Senthil Kumaran2, Vinay Goyal3, and Achal K Srivastava2
1IIT Delhi, Delhi, India, 2All India Institute of Medical Sciences, Delhi, India, 3Neuroscience Institute, Medanta-The Medicity, Delhi, India
1IIT Delhi, Delhi, India, 2All India Institute of Medical Sciences, Delhi, India, 3Neuroscience Institute, Medanta-The Medicity, Delhi, India
Synopsis
Repetitive transcranial magnetic stimulation is known to render clinical benefits in subjects with Parkinson’s Disease. Because of dopaminergic depletion the cortical connectivity patterns are affected in PD. This study aimed to inhibit the primary motor area which is an important node in the movement control pathway. The effect was studied using clinical scales and task based functional connectivity. The results reveal the ability of rTMS to facilitate the movement by inducting cortical as well as subcortical brain regions.
Introduction
Parkinson’s Disease (PD) is a progressive degenerative disorder causing difficulty with movement planning and execution. The disease occurs due to loss of dopaminergic neurons in substantia nigra and leads to loss of direct pathway of movement control. This causes alterations in cortical connectivity patterns1. Pharmacological interventions are known to restore the connectivity patterns. But whether newer intervention modalities act by restoring the connectivity patterns remains unclear2,3. These modalities like repetitive transcranial magnetic stimulation(rTMS) is known to impart motor clinical benefit4,5. This study was thus designed to explore the effect of 1Hz repetetive transcranial magnetic stimulation (rTMS) on task based functional connectivity in PD.Methods
A total of 13 subjects [age (mean ± sd) = 57.23 ± 8.02, duration of disease (mean ± sd) =5.92 ± 2.98] were recruited according to a pre-defined inclusion/exclusion criteria and all subjects underwent 4 sessions of sham sessions followed by real sessions. Sessions were conducted once a week. 3000 pulses were delivered at left Primary motor area during each session. Magstim Rapid 2 Plus (Magstim Co, Ltd, Wales, UK) stimulator was used with a 70 mm figure of eight a realistic sham coil (D70-AFC-3950) and real coil (D70-AFC-3910) for sham and real sessions respectively. MA was localized at C3 according to the 10-20 EEG system and the sessions were delivered at 100% resting motor threshold (RMT). Stimulator output eliciting a motor evoked potential (MEP) of 50μV in at least 5 out of 10 trials was the RMT. The outcomes (visuospatial BOLD task, UPDRS, PDQ39, PPB) were assessed at baseline, after sham sessions and after real sessions. A visuospatial BOLD task included a set of randomly appearing images of a corridor during the active blocks of the task. The images showed turns at the end of the corridor, with some images in which the turns appeared nearer and in some farther from the viewer’s perspective. Eight images were presented randomly (4 of the right turn and 4 of the left turn). Subjects had to respond whether the turn was towards the right or left by pressing a button with the respective hand. During the rest, a set of 4 images (appearing for 8 seconds each) were presented. The subjects were instructed not to respond during the rest sessions. Task was presented using the E-Prime software (version 1.0, Psychology Software Tools, Pittsburgh, PA, USA) and an E-sys IFIS system (Philips Medical Systems, Best, The Netherlands) (Schneider, Eschman, and Zuccolotto 2002). Subjects responded with a button press on an MRI compatible response pad (Lumina LP 400, Cedrus Inc., USA). Functional data were analysed using Conn toolbox (20.b) and clinical outcomes were assessed with SPSS ver. 22. Repeated measures anova was used to identify changes.Result
Decreased connectivity was observed between motor areas and parietal association areas at baseline and at sham. After real stimulation a significantly increased connectivity was observed between motor areas with parietal association and subcortical areas(Figure 1)UPDRS II (p<0.001), UPDRS III (p<0.001) along with Mobility (p<0.001) and activities of daily living-ADL (p<0.001), segments of PDQ 39 were significantly reduced(Figure 2). The dexterity performance showed significant increase in performance all segments of PPB [R(p=0.003), L(p=0.009), assembly(p=0.001)] (Figure 3).
Discussion
1 Hz TMS lead to clinical improvement and increased dexterity performance. The connectivity patterns show that these improvements could be due to enhanced cortical connectivity between motor and association areas as well subcortical regions. CONCLUSION:Conclusion
1Hz at Primary motor area imparts clinical benefits by facilitating cortico-cortical networks along with pallido-thalamic connectivity.Acknowledgements
No acknowledgement found.References
- Whone, A. L., Moore, R. Y., Piccini, P. P. & Brooks, D. J. Plasticity of the nigropallidal pathway in Parkinson’s disease. Ann. Neurol. (2003). doi:10.1002/ana.10427
- Udupa, K. & Chen, R. Motor Cortical Plasticity in Parkinson’s Disease. Front. Neurol. 4, (2013).
- Zhong, J. et al. Levodopa imparts a normalizing effect on default-mode network connectivity in non-demented Parkinson’s disease. Neurosci. Lett. 705, 159–166 (2019).
- Shirota, Y., Hamada, M. & Ugawa, Y. Clinical applications of rTMS in parkinson’s disease. in Therapeutic rTMS in Neurology: Principles, Evidence, and Practice Recommendations 129–145 (2015). doi:10.1007/978-3-319-25721-1_9
- Filipović, S. R., Rothwell, J. C. & Bhatia, K. Slow (1 Hz) repetitive transcranial magnetic stimulation (rTMS) induces a sustained change in cortical excitability in patients with Parkinson’s disease. Clin. Neurophysiol. (2010). doi:10.1016/j.clinph.2010.01.031
Figures
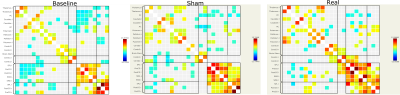
Figure 1. ROI to ROI
connectivity correlation matrix (RRC-matrix) at baseline, after sham
stimulations, after real stimulation.
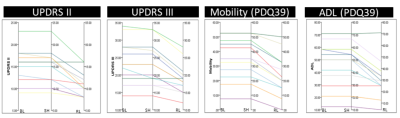
Figure 2. Change of clinical scores (UPDRS and PDQ-39 sub-segments).
Each colored line depicts single subject. BL-baseline, SH-sham, RL-real.
Decrease in score indicates clinical improvement.
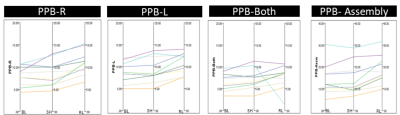
Figure 3. Change of scores with Purdue PegBoard dexterity performance.
Each colored line depicts single subject. BL-baseline, SH-sham, RL-real. Increase
in score indicates clinical improvement. PPB-R(purdue pegboard with right hand), PPB-L(purdue pegboard with left hand), PPB-Both (purdue pegboard with both hand), PPB-Assembly (purdue pegboard assembly making).
DOI: https://doi.org/10.58530/2022/3069