3028
The effect of total sleep deprivation under workload on spontaneous brain activity in medical staff: a resting-state functional MR imaging study
Cong Peng1, Ding bo Guo1, lisha Nie2, Liuheng Liu 1, Dongling Xiao 1, and Hua Yang1
1Chongqing Hospital of Traditional Chinese Medicine, Chongqing, China, 2GE Healthcare, MR Research China, Beijing, Chongqing, China
1Chongqing Hospital of Traditional Chinese Medicine, Chongqing, China, 2GE Healthcare, MR Research China, Beijing, Chongqing, China
Synopsis
The current study aims to assess the effect of total sleep deprivation (TSD) under workload on spontaneous brain activity in medical staff and to further investigate its latent associations with clinical markers. It was concluded that spontaneous brain activity abnormalities occurred during TSD under workload, which might explain the reduced performance of these participants on neurocognitive tests.
Introduction
TSD is a state of sleep loss resulting in physiological and psychological changes, and the decline of cognitive abilities. Lack of sleep has become a worldwide health problem [1]. Meta analysis showed that sleep deficit affects attention, working memory, processing speed, short-term memory and reasoning [2]. Lei et al. reported that alterations between salience network and default mode network might be critical in cognitive impairment after TSD [3]. The increasing demand for medical treatment, and various medical emergencies put forward higher requirements for medical staff. They may have to save life in the state of TSD, with mental fatigue. Therefore, it is important to explore the mechanism of TSD affecting cognition to predict and combat mental fatigue of medical staff. We hypothesized that TSD has a negative effect on resting-state spontaneous brain activity in medical staff. We selected resting-state functional MR imaging (rs-fMRI) with an amplitude of low-frequency fluctuations (ALFF) and regional homogeneity (ReHo) algorithm to measure intrinsic brain responses, to explore the changes of brain spontaneous activity from multi algorithms. The purpose of this study was to analyze the spontaneous brain activity patterns in medical staff with TSD by using rs-fMRI with ALFF and ReHo algorithm, and to further investigate its latent associations with clinical markers.Material and Methods
Thirty-six medical staff before and after TSD were examined by 3.0T MRI scanner(Architect, GE Healthcare, Waukesha, USA) using rs-fMRI. The exclusion criteria as follows: (1) brain lesions, such as severe craniocerebral trauma, stroke, and brain tumor; (2) drug or alcohol abuse; and (3) psychiatric issues. We used fractional ALFF (fALFF) and regional homogeneity (ReHo) to explore the brain activity changes in TSD subjects. Based on the brain regions with significant changes in fALFF and ReHo as ROI, we used functional connectivity (FC) to detect the potential abnormal brain function changes in TSD subjects, and the Pearson correlation analysis was made with the neuropsychological test. P<0.05 was considered statistically significant.Results
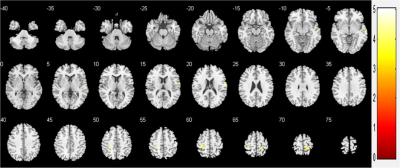
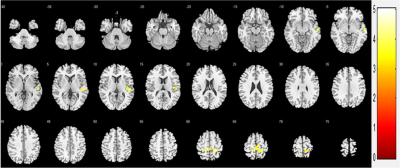
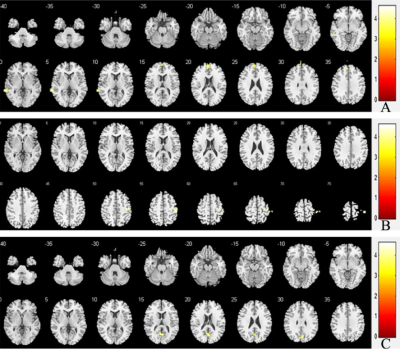
According to the analysis of fALFF, the brain activities of the right superior temporal gyrus, bilateral postcentral gyrus were significantly enhanced after TSD (p<0.05, FDR corrected at the cluster level, initial voxel-wise threshold p=0.001) (Figure 1). According to the analysis of ReHo, the ReHo values of the right superior temporal gyrus, bilateral postcentral gyrus increased after TSD (p<0.05, FDR corrected at the cluster level, initial voxel-wise threshold p=0.001) (Figure 2). Using right superior temporal gyrus as the seed point, the FC of left medial superior frontal gyrus and Left middle temporal gyrus were significantly enhanced after TSD (p<0.05, FWE corrected at the cluster level, initial voxel-wise threshold p=0.001) (Figure 3A). Using right central posterior gyrus as the seed point, the FC of right precentral gyrus was significantly enhanced after TSD (p<0.05, FWE corrected at the cluster level, initial voxel-wise threshold p=0.001) (Figure 3B). Using left postcentral gyrus was used as the seed point, the FC of left precuneus was significantly enhanced after TSD (p<0.05, FWE corrected at the cluster level, initial voxel-wise threshold p=0.001) (Figure 3C). We also found that the FC value of the left medial superior frontal gyrus was positively correlated with scores of Digit symbol test, negatively correlated with scores of Number connecting A test and Serial dotting test, and the FC value of the right precentral was negatively correlated with scores of Serial dotting test (table 4).Discussion and Conclusion
The results found that after TSD, both ALFF and ReHo subjects had increased spontaneous brain activity in bilateral posterior central gyrus and right superior temporal gyrus. ALFF directly reflected the intensity of brain activity, and ReHo indirectly reflected brain functional activity. The overlap of brain regions obtained by the two algorithms greatly enhances the persuasion. The increase of spontaneous activity of posterior central gyrus is related to the decrease of sleep quality and the increase of anxiety[4,5]. The FC with the whole brain was made by taking the brain regions with changed spontaneous brain activity as the seed point. The FC enhanced after TSD. Most of these brain regions were located in the default mode network. At the same time, some brain regions with enhanced FC may be related to the performance of neuropsychological test. It was concluded that spontaneous brain activity abnormalities occurred during TSD under workload, which might explain the reduced performance of these participants on neurocognitive tests.Acknowledgements
Our team thank all medical staff for their participation.References
[1] Basner M, Rao H, Goel N, et al. Sleep deprivation and neurobehavioral dynamics. Curr Opin Neurobiol. 2013,23(5):854-863. [2] Lim J, Dinges DF. A meta-analysis of the impact of short-term sleep deprivation on cognitive variables. Psychol Bull2010;136:375–389. [3] Lei Y, Shao Y, Wang L, et al. Large-scale brain network coupling predicts total sleep deprivation effects on cognitive capacity. PloSone.2015.10(7), e0133959. [4] Zhou F, Huang S, Zhuang Y, et al. Frequency-dependent changes in local intrinsic oscillations in chronic primary insomnia: A study of the amplitude of low-frequency fluctuations in the resting state [J]. Neuroimage Clin.2016,15:458-465. [5] Gao L, Bai LJ, Zhang YC, et al. Frequency-dependent changes of local resting oscillations in sleep-deprived brain. PLoS ONE. 2015,10(3),1-15.
DOI: https://doi.org/10.58530/2022/3028