2999
Thalamus regulates emotional performance in different pathways with CSVD involved
Bei Wang1, Cen Guo2, He Wang1,3, Yan Han2, and Ying-Hua Chu4
1Institute of Science and Technology for Brain-Inspired Intelligence, Fudan University, Shanghai, China, 2Department of Neurology, Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai, China, 3Human Phenome Institute, Fudan University, Shanghai, China, 4MR Collaboration, Siemens Healthineers Ltd., Shanghai, China
1Institute of Science and Technology for Brain-Inspired Intelligence, Fudan University, Shanghai, China, 2Department of Neurology, Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai, China, 3Human Phenome Institute, Fudan University, Shanghai, China, 4MR Collaboration, Siemens Healthineers Ltd., Shanghai, China
Synopsis
With the help of 7T Imaging, we investigated the association between the thalamic anterior vascularization patterns and emotions, including depression and anxiety. Cerebral small vessel diseases were considered as a risk factor for emotional performance. The thalamic anterior vascularization pattern was found association with depression and anxiety in subjects without CSVD burden. In the CSVD group, the thalamic volume and cortex thickness in pars triangularis, rostral middle frontal and superior frontal were found significantly correlated with both HAMD and HAMA test scores. It suggests the pathway of the thalamus regulating emotion changes with the development of CSVD.
Introduction
The thalamus, which has connections to most regions in the cerebral cortex, midbrain, and cerebellum, is composed of over a hundred nuclei that each serve a unique role, ranging from regulating sensory, motor functions, as well as emotion and consciousness [1]. A sufficient blood supply is important in maintaining regular function. However, little is known about the association between the richness of thalamus vascular supply and thalamic function due to the invisible of responsible vessels in conventional MRI. With the help of 7T MRI, the thalamic vascularization patterns in adults were classified in vivo firstly. The anatomic variation in thalamic blood supply mainly happens in the anterior vascular territory, and infarction in this territory was reported involving emotional disturbance [2]. The thalamic anterior vascularization pattern can be categorized into a mixed supply from both the tuberothalamic artery and paramedian arteries, or a single supply from either the tuberothalamic artery or the paramedian arteries. We hypothesized that thalamic anterior vascularization pattern may be associated with emotional performance and structural changes. Additionally, the interruption of cerebral small vessel diseases (CSVD) was considered a grouping variable in further study.Methods
Participants44 adults aged from 25 to 75 were included in the study. Participants were excluded if they had previous cardiovascular or cerebrovascular events, renal dysfunction, or metabolic disease including diagnosis of familial hyperlipidemia. A secondary exclusion criterion was any MRI-revealed brain lesions, except for CSVD. Participants were separated into two groups: the CSVD group (17 adults) and the control group (27 adults).
MRI Acquisition
All participants underwent a 7T ultrahigh-field MRI scan (MAGNETOM Terra, Siemens Healthcare, Erlangen, Germany) using a 32-channel head-coil with the following sequences: T1 imaging with MP2RAGE (voxel size = 0.7x0.7x0.8mm, TR = 3800ms, TE = 2.27ms, TI1 = 800ms, TI2 = 2700ms, flip angle1 = 7°, flip angle2 = 5°); T2 dark-fluid imaging (voxel size of 1.1x1.1x1.0mm, TR = 9000ms, TE = 270ms, TI = 2600ms); TOF imaging (voxel size = 0.35x0.35x1mm, TR = 20ms, TE = 4.34ms, flip angle = 18°).
Image Processing
All MRI scans were reviewed for quality before analysis. Subjects with motion artifacts were excluded.
To locate the thalamus precisely, white-matter-nulled (WMn) contrast images [3] were synthesized from T1 maps using the following equation:
Msyn = M0(1-2eTI/T1)
Where = 1 and TI was set to 670ms to suppress the signal of white matter and improve the contrast of the thalamic boundaries. Then, automatic registration and manual correction were complete based on the WMn contrast images to get the thalamic masks and thalamic volumes. The thalamic masks were transformed to corresponding TOF space by registering the T1 image to TOF of individuals rigidly.
All the registrations were completed using Advanced Normalization Tools (ANTs) (https://github.com/ANTsX/ANTs).
The region of interest was determined by overlaying the thalamic masks on TOF images in MRIcron. As the anatomic variation happens in hemispheres in the same subject, we define a single blood supply pattern if a single supply happens in the thalamus on both sides.
Frontal cortex thickness, which is reported relating to emotional performance [7], were assessed using FreeSurfer (https://surfer.nmr.mgh.harvard.edu).
Scale Tests
For all participants, depression and anxiety were assessed using Hamilton Depression Scale (HAMD) and Hamilton Anxiety Scale (HAMA), respectively. The total CSVD burden on brain MRI was assessed by a clinical specialist [4,6].
Statistics
Correlation analysis was used to evaluate the correlation between vascular patterns and emotional performance in each group. Age and sex were always included as covariates. P<0.05 was considered statistically significant in all analyses.
Results and Discussion
The average age in the CSVD group is significantly higher, which is consistent with previous works [5]. There was no correlation between the thalamic anterior vascular patterns and thalamic volume in both groups.In the CSVD group, no correlation was found between the thalamic anterior vascular patterns and HAMD, HAMA test scores. However, the thalamic volume and cortex thickness in pars triangularis, rostral middle frontal and superior frontal in both hemispheres were found significantly correlated with both HAMD and HAMA test scores. Moreover, the thalamic volume also associated with cortex thickness in above three areas, which suggested a mediation effect.
Interestingly, we found that the emotional performance only associated with the vascular patterns in control group, which was entirely different from the CSVD group. It may suggest that the pathway of the thalamus regulating emotion changes with the development of CSVD.
Conclusion
The thalamus regulates emotions in different pathways. Mixed vascular supply pattern can help with the emotional performance in people with no CSVD burden. With CSVD concern, thalamic volume and related cortex thickness are more important for regulating emotions.Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 81971583), National Key R&D Program of China (No. 2018YFC1312900), Shanghai Natural Science Foundation (No. 20ZR1406400), Shanghai Municipal Science and Technology Major Project (No.2017SHZDZX01, No.2018SHZDZX01) and ZJLab.References
- Bordes S, Werner C, Mathkour M, McCormack E, Iwanaga J, Loukas M, Lammle M, Dumont AS, Tubbs RS. Arterial Supply of the Thalamus: A Comprehensive Review. World Neurosurg. 2020 May;137:310-318. doi: 10.1016/j.wneu.2020.01.237. Epub 2020 Feb 7. PMID: 32036065.
- Child ND, Benarroch EE. Anterior nucleus of the thalamus: functional organization and clinical implications. Neurology. 2013 Nov 19;81(21):1869-76. doi: 10.1212/01.wnl.0000436078.95856.56. Epub 2013 Oct 18. PMID: 24142476.
- Datta R, Bacchus MK, Kumar D, Elliott MA, Rao A, Dolui S, Reddy R, Banwell BL, Saranathan M. Fast automatic segmentation of thalamic nuclei from MP2RAGE acquisition at 7 Tesla. Magn Reson Med. 2021 May;85(5):2781-2790. doi: 10.1002/mrm.28608. Epub 2020 Dec 3. PMID: 33270943.
- Staals J, Makin SD, Doubal FN, Dennis MS, Wardlaw JM. Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden. Neurology. 2014 Sep 30;83(14):1228-34. doi: 10.1212/WNL.0000000000000837. Epub 2014 Aug 27. PMID: 25165388; PMCID: PMC4180484.
- Li T, Huang Y, Cai W, Chen X, Men X, Lu T, Wu A, Lu Z. Age-related cerebral small vessel disease and inflammaging. Cell Death Dis. 2020 Oct 30;11(10):932. doi: 10.1038/s41419-020-03137-x. PMID: 33127878; PMCID: PMC7603301.
- Clancy U, Gilmartin D, Jochems ACC, Knox L, Doubal FN, Wardlaw JM. Neuropsychiatric symptoms associated with cerebral small vessel disease: a systematic review and meta-analysis. Lancet Psychiatry. 2021 Mar;8(3):225-236. doi: 10.1016/S2215-0366(20)30431-4. Epub 2021 Feb 1. PMID: 33539776.
- Li Q, Zhao Y, Chen Z, Long J, Dai J, Huang X, Lui S, Radua J, Vieta E, Kemp GJ, Sweeney JA, Li F, Gong Q. Meta-analysis of cortical thickness abnormalities in medication-free patients with major depressive disorder. Neuropsychopharmacology. 2020 Mar;45(4):703-712. doi: 10.1038/s41386-019-0563-9. Epub 2019 Nov 6. Erratum in: Neuropsychopharmacology. 2019 Dec 12;: PMID: 31694045; PMCID: PMC7021694.
Figures
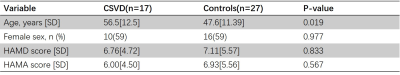
Demographics
of
the
sample.Independent sample t-test or x2
– test were conducted. P-values < 0.05 were considered statistically significant.
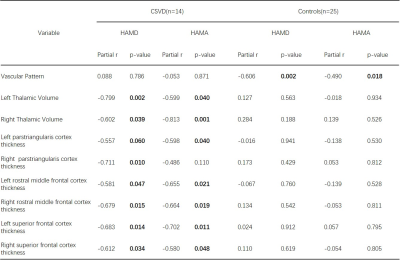
Associations between the thalamic anterior vascular pattern, thalamic volume, frontal cortex thickness and emotion performance in CSVD and control group. All the correlation analyses were adjusting for age and sex. 3 CSVD and 2 control subjects were removed for lacking of cortex thickness information.
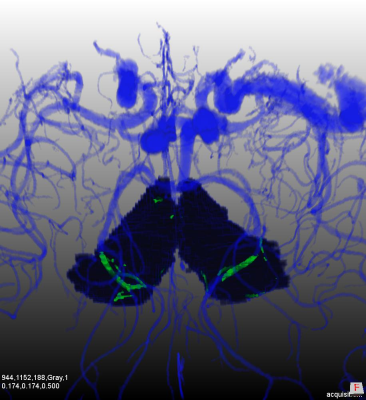
Thalamic vascularization pattern shown in 7T. Left in the figure is a mixed supply pattern, and right in the figure is a single supply pattern.
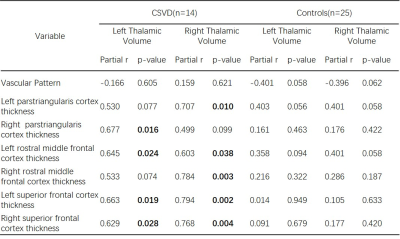
Associations between the thalamic anterior vascular pattern, frontal cortex thickness and thalamic volume in CSVD and control group. All the correlation analyses were adjusting for age and sex. 3 CSVD and 2 control subjects were removed for lacking of cortex thickness information.
DOI: https://doi.org/10.58530/2022/2999