2979
Feasibility of 3D-MENSA sequence for qualitative assessment of lumbosacral plexus nerve root in comparison with 3D-MERGE MRI1Tongji Hospital,Tongji Medical College,Huazhong University of Science and Technology, Wuhan,China, China, 2GE Healthcare, Beijing, China., China
Synopsis
Lumbar radiculopathy is a worldwide cause of disability. Mechanical compression of nerve root may lead to nerve inflammatory changes. Peripheral blood vessels overlapping with inflammatory changes can make radiologists confused and result misdiagnosis. To differ lesions from vessels in lumbosacral plexus nerve imaging, three-dimensional motion-sensitized driven equilibrium prepared rapid gradient echo (3D-MERGE) and three-dimensional multiecho in the steady-state acquisition (3D-MENSA) were investigated. Our study showed 3D-MENSA images showed greater nerve-to-vein CNR and CR than 3D-MERGE and the measurement repeatability of the same observer was good. Overall, 3D-MENSA sequence provided images with superior vascular suppression and offered better conspicuity of LSP.
Introduction
Lumbar radiculopathy remains a clinical challenge to primary care clinicians in both assessment and diagnosis. Misdiagnosis and inappropriate treatment to patients cause poor health outcomes, exacerbating existed weakness condition.1 Mechanical compression of the nerve root may alter the intra-radicular circulation, produce nerve fiber dysfunction and lead to a series of pathological changes in intra-neurial tissue, including edema formation, demyelination, and fibrosis.2 When inflammatory changes such as nerve edema overlap with peripheral blood vessels, radiologists may feel confused and make misdiagnosis such as neuropathy. Three-dimensional motion-sensitized driven equilibrium prepared rapid gradient echo (3D-MERGE) is used for blood vessel wall imaging because of its excellent vascular suppression3 while three-dimensional 3D multiecho in the steady-state acquisition (3D-MENSA)4 had better vascular suppression in lumber nerve imaging in our pre-study. Therefore, we aimed to investigate the feasibility of 3D-MENSA for lumbosacral plexus imaging using 3D-MERGE as reference standard.Methods
This study was approved by the institutions review board of our hospital. 11 volunteers (ten women, mean age was 22 years, ranged 21-25 years; one man, aged 22 years) were recruited. All volunteers underwent conventional sequence , and MENSA and MERGE sequences on 3.0 T MRI system (Signa Pioneer, GE Healthcare, Milwaukee, USA) with a body coil and bed spine coil. The main parameters of 3D-MENSA and 3D-MERGE were acquired with the same voxel size of 1*1*1mm but different scan time (4 mins 16 secs; 4 minutes 46 secs). Maximum intensity projection (MIP) images of each original scanned images were assessed after post-processing. The First sacral nerve root and its surrounding tissues including muscles, fat, iliac vein, the first sacral body and background air were selected as regions of interest (ROI), and then the signal-to-noise ratio (SNR), contrast-to-noise ratio (CNR) and contrast ratio (CR) were calculated by a radiologist and repeated the measurements two weeks later. A paired t-test was used to assess differences of parameters for 3D-MENSA and 3D-MERGE images, and the measurement repeatability of the same observer was tested using the intra-class correlation coefficient (ICC). All statistical analyses were performed using SPSS 20.0 software.Results
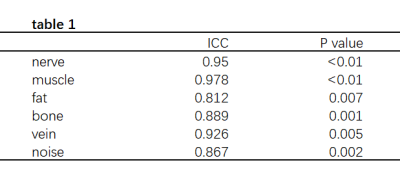
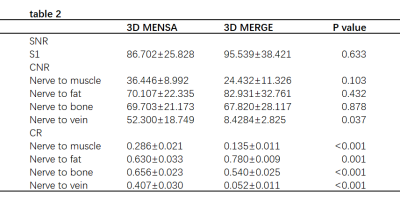
The measurement repeatability of the same observer was good (table 1). 3D-MENSA images showed no significant difference SNR compared to 3D-MERGE images (86.70±25.83 versus 95.54±38.42;p=0.633). 3D-MENSA images showed greater nerve-to-vein CNR compared to 3D-MERGE images (52.30 ±18.74 versus 8.43±2.83, p=0.037). However, no significant differences were observed in nerve-to-bone (p=0.878) and nerve-to-fat (p=0.432) and nerve-to-muscle (p=0.103) CNRs between two kinds of images. Moreover, 3D-MENSA images showed significantly higher CR of nerves to surrounding vascular structures (0.41±0.03 versus 0.05±0.01, p<0.001), bones (0.66±0.02 versus 0.54±0.03, p<0.001), fat tissues (0.63±0.032 versus 0.78±0.009, p=0.001), muscles (0.29±0.021 versus 0.14±0.01, p<0.001) than 3D-MERGE images (Table 2).Discussion
This is the first study to assess performance of MENSA and MERGE techniques on the diagnosis of lumbosacral plexus nerve and explore clinical feasibility and reproducibility of measurements. 3D-MENSA is a technique that averages 2 echoes acquired within the same repetition time (TR) to elevate fluid signal and can also acquire two separate images to assess signal changes of lesions by optimizing protocol. 4 3D-MERGE has large coverage and short scan time for carotid vessel wall imaging. Previous studies have showed excellent agreement on measurements of luminal stenosis between 3D-MERGE and digital subtraction angiography. 5 However, our research showed that high-resolution 3D MENSA provides better blood vessel suppression in lumbosacral plexus nerve root imaging than 3D-MERGE, which almost completely eliminates the interference of peripheral blood vessels (Figure 1).For the Imaging quality assessment, CR indicates the relative difference between signals from different tissues, while CNR represents the ratio of the absolute difference between two tissue signals and noise. 6 3D-MENSA with higher nerve-to-vein CNR and CRs displayed sharp image in details and achieved excellent gray-level. Both 3D techniques can be used to constructed MIP (maximum intensity projection) images which reduce the partial volume artifact due to scanning in thin continuous slices. Other than strength beyond high nerve-to-vein contrast-to-noise ratio (CNR), 3D-MENSA has higher time resolution ( 4 mins 16 secs VS 4 minutes 46 secs) that relieves the pressure on radiologists. In our preliminary study, diagnostic efficacy of 3D-MENSA MR sequence on lumbosacral plexus nerve imaging has not been explored, so further research will focus on the diagnostic performance in lumbar radiculopathy.
Conclusion
3D-MENSA sequence provided images with superior vascular suppression and thus offered better conspicuity of LSP. This may greatly benefit to patients who experience traumatic LSP lesions when clinicians make diagnosis and treatment plans.Acknowledgements
We thank for the support of the National Natural Science Foundation of China (NSFC) (No.31630025 and 81930045)References
1.Tawa N, Rhoda A, Diener I. Accuracy of clinical neurological examination in diagnosing lumbo-sacral radiculopathy: a systematic literature review. BMC Musculoskelet Disord. 2017 Feb 23;18(1):93.2.Kobayashi S, Yoshizawa H, Yamada S. Pathology of lumbar nerve root compression. Part 1: Intraradicular inflammatory changes induced by mechanical compression. J Orthop Res. 2004 Jan;22(1):170-9.
3.Baylam Geleri D, Watase H, Chu B, et,al . Detection of Advanced Lesions of Atherosclerosis in Carotid Arteries Using 3-Dimensional Motion-Sensitized Driven-Equilibrium Prepared Rapid Gradient Echo (3D-MERGE) Magnetic Resonance Imaging as a Screening Tool. Stroke. 2021 Sep 30:STROKEAHA120032505.
4.Chen CA, Kijowski R, Shapiro LM, et.al. Cartilage morphology at 3.0T: assessment of three-dimensional magnetic resonance imaging techniques. J Magn Reson Imaging. 2010 Jul;32(1):173-83.
5.Murata K, Murata N, Chu B, et,al ; CARE-II Study Collaborators. Characterization of Carotid Atherosclerotic Plaques Using 3-Dimensional MERGE Magnetic Resonance Imaging and Correlation With Stroke Risk Factors. Stroke. 2020 Feb;51(2):475-480.
6. Zhang Y, Kong X, Zhao Q, et,al. Enhanced MR neurography of the lumbosacral plexus with robust vascular suppression and improved delineation of its small branches. Eur J Radiol. 2020 Aug;129:109128.
Figures