2941
Post-Therapy cortical normalization for phonological processing in developmental dyslexia1Dept. of NeuroRehab, speech therapy and audiology, Escorts Heart Institute and Research Center, New Delhi, India, 2Former Dept. of NMR & MRI Facility, All India Institute of Medical Sciences, New Delhi, India, 3Former Dept. of Psychiatry (Psychology Unit), All India Institute of Medical Sciences, New Delhi, India, 4Dept. of Psychiatry, All India Institute of Medical Sciences, New Delhi, India, 5Dept. of Neurology, Fortis Hospital, Vasant Kunj, New Delhi, India, 6Former Dept. of Neurology, All India Institute of Medical Sciences, New Delhi, India, 7Former Dept. of Linguistics, School of Language, Literature and Culture Studies, Jawaharlal Nehru University, New Delhi, India, 8Dept. of Biostatistics, All India Institute of Medical Sciences, New Delhi, India, 9Dept. of NMR & MRI Facility, All India Institute of Medical Sciences, New Delhi, India
Synopsis
Dyslexia is a neurodevelopmental disorder with complex spectrum and continuum of cognitive deficits leading to academic and emotional life-long burden, so optimal remediation becomes essential and challenging. Pre- and post- functional imaging studies show the recovery changes in brain with rehabilitation, but can fMRI biomarkers be explored and utilized for customizing therapeutic strategies in dyslexia. In present study at baseline we randomly allocated dyslexic children to therapy (Rx) and waitlist (nonRx) groups. Based on the potential (positive and negative) neural-markers at baseline, we tailored cognitive modules for phonological intervention. Remediation resulted in improved performance and cortical normalization
Background
Reading-writing has specialized cortical architecture and problem may lead to neurodevelopment disorder1,2,3. Children and adolescents with dyslexia have spectrum of deficits involving phonological-processing, reading, spelling, writing, working-memory and executive problems4,5,6,7. It’s reported that neural deficits may not directly reflect in behavior, and evidence-based interventions are critically needed6,8. Hence in this study therapy was tailored on neural-markers and remedial gains were measured as cortical normalization.Methods
After ethical approval 30 participants were randomly allocated to two groups Group A (therapy, Rx) and Group B (wait-list, nonRx). Assessments were done at baseline and follow-up. Intervention for group A was “tailored” based on (baseline) potential ‘biomarkers’ (negative and positive) evaluated with behavior plus task evoked functional magnetic resonance imaging (task-fMRI). FMRI carried out on 3T MR scanner (Achieva 3.0T TX, M/s. Philips Healthcare, Amsterdam, The Netherlands) with 32-channel head coil (head supported and immobilized). Paradigm used was English meaningful-words and pseudowords. The stimuli were presented using E-prime (version 1.1, Psychology Software Tools Inc, USA) and MR compatible LCD monitor synced with ESys fMRI System, Invivo Corp, M/s. Philips Healthcare. fMRI (blood oxygenation level dependent activity, BOLD) acquired using multi-slice T2* GE-EPI sequence with parameters FOV 230mm, 31 slices, slice thickness 5 mm (without slice gap), TR 2s, dynamics 222 and total acquisition time 444s. Therapeutic strategies consisted of cognitive training modules shared in 22 to 24 clinical sessions over six months duration. Data of three therapy group children and two non-therapy was excluded due to head-motion in fMRI images. So to balance two-groups final analysis of twenty-four participants’ (Rx n=12; nonRx n=12) was done with SPSS (behavioral performance) and SPM12 (fMRI)Result and Discussion
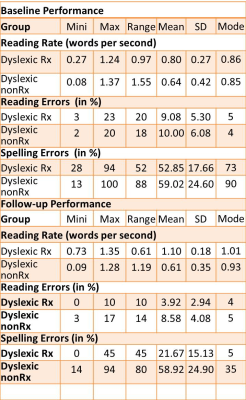
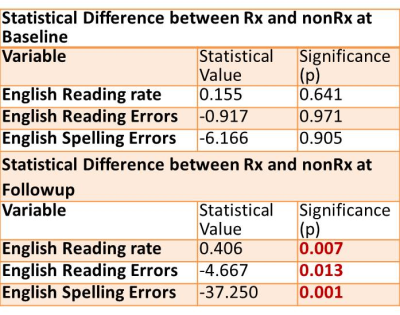
Performance group differences at baseline and follow-up are shown in Table-1. Follow-up analysis showed significant improvement in reading, spelling, writing errors in Rx group compared to nonRx (Table-2). Rx Group Baseline meaningful words induced activity in left postcentral gyrus, cingulate (BA 24), middle frontal (BA 6), bilateral insula. Follow-up activity was observed in bilateral fusiform (BA 37), left inferior occipital (BA 17), right inferior frontal (BA 47), middle frontal (BA 6) and anterior cingulate (BA 32) showing cortical reorganization post therapy1,8,10. In group B (nonRx) follow-up activity was in right insula (123 parietal voxels), precuneus (133 parietal voxels, 12 occipital voxels), cuneus (10 voxel-clusters) and bilateral frontal (right superior, middle frontal and left BA 46) suggestive of compensatory mechanism9. In nonRx group follow-up activation in left superior temporal (BA 22) indicates natural linguistic learning1.Conclusion
Therapy induced significant improvement in performance with BOLD activity in fusiform, inferior occipital (BA 17) and inferior frontal (BA 47) for meaningful visual word processing (compared to pseudowords) show cortical normalization for phonological processing.Acknowledgements
No acknowledgement found.References
[1]Centanni TM, Norton ES, Ozernov-Palchik O, et al. Disrupted left fusiform response to print in beginning kindergartners is associated with subsequent reading. Neuroimage Clin. 2019;22:101715. doi:10.1016/j.nicl.2019.101715
[2]Démonet JF, Taylor MJ, Chaix Y. Developmental dyslexia. Lancet 2004; 363: 1451–1460. https://www.chu-toulouse.fr/IMG/pdf/Demonet_et_al_2004-2.pdf
[3]Raschle NM, Zuk J, Gaab N. Functional characteristics of developmental dyslexia in left-hemispheric posterior brain regions predate reading onset. Proc Natl Acad Sci U S A. 2012;109(6):2156-2161. doi:10.1073/pnas.1107721109
[4]Ramus F, Rosen S, Dakin SC, Day BL, Castellote JM, White S, Frith U. Theories of developmental dyslexia: insights from a multiple case study of dyslexic adults. Brain, 2003;126(4):841–865. https://doi.org/10.1093/brain/awg076
[5]Snowling MJ. Phonological processing and developmental dyslexia. J Research in Reading, 1995;18(2): 132–138. https://doi.org/10.1111/j.1467-9817.1995.tb00079.x
[6]Snowling MJ, Hayiou-Thomas ME, Nash HM, Hulme C. Dyslexia and developmental language disorder: comorbid disorders with distinct effects on reading comprehension. J Child Psychol Psychiatry. 2020;61(6):672-680. doi:10.1111/jcpp.13140
[7]Toffoli L, Scerif G, Snowling MJ, Norcia AM, Manning C. Global motion evoked potentials in autistic and dyslexic children: A cross-syndrome approach. Cortex. 2021;143:109-126. doi:10.1016/j.cortex.2021.06.018
[8]Eden GF, Jones KM, Cappell K, et al. Neural changes following remediation in adult developmental dyslexia. Neuron. 2004;44(3):411-422. doi:10.1016/j.neuron.2004.10.019
[9]Yan X, Jiang K, Li H, Wang Z, Perkins K, Cao F. Convergent and divergent brain structural and functional abnormalities associated with developmental dyslexia. Elife. 2021;10:e69523. Published 2021 Sep 27. doi:10.7554/eLife.69523
[10]Wang J, Yamasaki BL, Weiss Y, Booth JR. Both frontal and temporal cortex exhibit phonological and semantic specialization during spoken language processing in 7- to 8-year-old children. Hum Brain Mapp. 2021;42(11):3534-3546. doi:10.1002/hbm.25450
Figures