2888
Quantitative Evaluation Of Potential L5/S1 Spinal Nerve Degeneration In LSTV With Bertolotti's Syndrome By Diffusion Tensor Imaging1The First Affiliated Hospital of Nanjing Medical University, Nanjing, China, 2GE Healthcare, MR Research, Beijing, China
Synopsis
This study aims to investigate if quantitative MR diffusion tensor imaging (DTI) technology can be applied to quantitatively evaluate the potential L5/S1 spinal nerve degeneration in patients with lumbosacral transitional vertebrae. By quantitative evaluating 52 patients, we found the L5/S1 spinal nerves' DTI FA values showed lower in type Ⅱ-Ⅳ LSTV cases while the nerves run through the bony articulation between the vertebra and sacrum. Therefore , quantitative MR DTI has a good performance for quantitative diagnosis of LSTV with Bertolotti's syndrome.
INTRODUCTION
Lumbosacral transitional vertebrae (LSTV) is congenital spinal anomaly defined as either sacralization of the lowest lumbar segment or lumbarization of the most superior sacral segment of the spine1, 2. Bertolotti's syndrome is the association of low back and lumbosacral radiculopathy with LSTV3. As the L5/S1 spinal nerves run through the bony articulation between the vertebra and sacrum, potential spinal nerve degeneration could occur by hidden compression, which is difficult to detect by routine radiographic examination3, 4. This study's main goal was to investigate if quantitative MR diffusion tensor imaging (DTI) technology can be applied to quantitatively evaluate the potential L5/S1 spinal nerve degeneration in patients with LSTV.METHODS
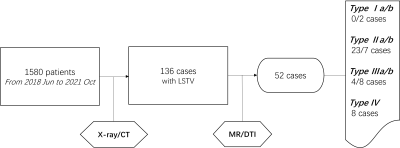
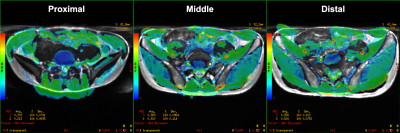
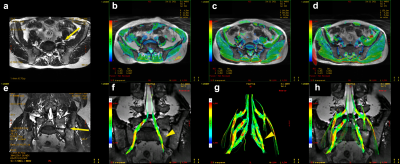
Subjects A total of 136 cases with lumbosacral transitional vertebrae were collected from 1580 hospitalized patients who were clinically diagnosed with lumbosacral radiculopathies between June 2018 and October 2021. The exclusion criteria were a history of spinal surgery, trauma, infection, neurological disease, lumbar disc herniation, extraforaminal stenosis compressed by disc bulging or a contraindication to MR imaging, such as metallic implants (not limited to the spine). After these exclusions, 52 cases (28 men, age: 47.4±15.4 years; 24 women, age: 55.9±15.9 years) were finally included in this study (Fig. 1). MRI imaging protocol Lumbar spinal MRI was performed on a 3.0 T MR scanner (Discovery 750w, GE Healthcare) with a 16-channel body coil. Conventional lumbar MRI protocol was performed, including axial T2WI fast spin-echo sequence, sagittal T2WI fast spin-echo, and T1WI sequences. T2 3D Cube sequences (TR/TE, 2040/128 ms) were obtained angled on the lumbosacral plexus. Based on the anatomical imaging mentioned above, DTI sequence was performed for L4 to S1 nerve roots with the following parameters: TR/TE, 6000/80 ms; MPG applied in 11 directions; FOV, 420 mm × 420 mm; matrix size, 96 × 128; voxel size, 4.38 mm × 3.28 mm × 4.0 mm; calculated voxel size, 1.64 mm × 1.64 mm × 4.0 mm; NEX, 4; slice number, 60; slice thickness, 4mm; slice gap, 0; b-value, 800s/mm2. Data analysis The classifications of lumbosacral transitional vertebrae were assessed by conventional lumbar MR and T2 3D Cube MR sequences. DTI data were processed with DTI post-processing software embedded into the Functool platform at a GE workstation (Advantage workstation 4.6; GE Medical Systems). DTI derived FA parametrical mappings were obtained correspondingly on the fusion image with axial T2-weighted images. The regions of interest (ROIs) were placed at proximal, middle and distal sub-regions, corresponding to the lateral recesses zone, the middle zone of the extended foramen and the extraforaminal zone of the nerve roots (Fig. 2). Statistical analysis Descriptive statistics were listed in the form of mean and standard deviation. SPSS 25.0 software was used to perform statistical analysis. The statistical figures were drawn using Graphpad Prism 8.0. The embedded t-test toolbox was applied to respectively compare the FA values of nerves that ran through the bony articulation between the vertebra and sacrum and the normal side in different types of LSTV cases.RESULTS
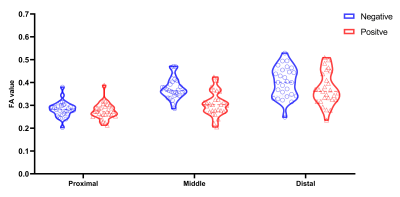
The Castellvi classifcation was used to classify the 52 included cases with LSTV as type Ⅰa/b (n=0/2), type Ⅱa/b (n=23/7), type Ⅲa/b (n=4/8), type Ⅳ (n=8) (Fig. 1). In unilateral typeⅡ- Ⅲ LSTV cases, the nerves' lower FA values were observed at the transitional side from proximal to distal sub-regions (p<0.005, Fig. 3). Meanwhile, in bilateral typeⅠ-Ⅲ LSTV cases, no significant difference in the FA values of the nerves was found on both sides at the transitional level. In type Ⅳ cases, only the middle sub-regions had lower FA values at type II transition side than type Ⅲ transition side (p<0.005). In type Ⅱ-Ⅳ cases,comparable FA values were found between type II transition side (n=45) and type Ⅲ(n=28) transition side of the nerves at all sub-regions. The visual DTI tractography abnormalities of nerves were found at the transition side and mainly at the middle sub-regions (Fig. 4).DISCUSSION
Most of the literature supports Bertolotti syndrome, the implicated transitional segments are Castellvi types II-IV2, 5. In this study, after excluding other routine factors for spinal nerve compression, the L5/S1 spinal nerves' DTI FA values showed lower in type Ⅱ-Ⅳ LSTV cases while the nerves run through the bony articulation between the vertebra and sacrum. The result indicates that potential L5/S1 spinal nerve degeneration in patients with LSTV exist in extended foramen composed by the enlarged transverse process that has a diarthrodial joint between itself and the sacrum (type Ⅱ)or complete osseous fusion of the transverse process to the sacrum (type Ⅲ) unilaterally or bilaterally. Quantitatively decreased DTI FA changes are reliable imaging findings in LSTV with Bertolotti's syndrome.CONCLUSION
Based on L5/S1 spinal nerve degeneration existing in extended foramen with LSTV, quantitative MR DTI has a good performance for quantitative diagnosis of LSTV with Bertolotti's syndrome.Acknowledgements
No acknowledgement found.References
1. Konin GP, Walz DM. Lumbosacral Transitional Vertebrae: Classification, Imaging Findings, and Clinical Relevance. Am J Neuroradiol. 2010;31(10):1778-86.
2. Jancuska JM, Spivak JM, Bendo JA. A Review of Symptomatic Lumbosacral Transitional Vertebrae: Bertolotti's Syndrome. International journal of spine surgery. 2015;9:42.
3. Kanematsu R, Hanakita J, Takahashi T, Minami M, Tomita Y, Honda F. Extraforaminal entrapment of the fifth lumbar spinal nerve by nearthrosis in patients with lumbosacral transitional vertebrae. Eur Spine J. 2020;29(9):2215-21.
4. Bahadir Ulger FE, Illeez OG. The Effect of Lumbosacral Transitional Vertebrae (LSTV) on Paraspinal Muscle Volume in Patients with Low Back Pain. Acad Radiol. 2020;27(7):944-50.
5. Jancuska JM, Spivak JM, Bendo JA. A Review of Symptomatic Lumbosacral Transitional Vertebrae: Bertolotti's Syndrome. Int J Spine Surg. 2015;9:42.
Figures