2834
Investigation of multiplexed sensitivity encoding diffusion-weighted imaging (DWI) in cervical carcinoma:comparison with conventional DWI
Tiebao Meng1, Weijing Zhang2, Haoqiang He2, Huiming Liu2, Guixiao Xu2, Fengting Zhu2, Long Qian3, and Chuanmiao Xie2
1Department of Radiology, Sun Yat-Sen University Cancer Center, Guangzhou, China, 2Sun Yat-Sen University Cancer Center, Guangzhou, China, 3GE Healthcare, Beijing, China
1Department of Radiology, Sun Yat-Sen University Cancer Center, Guangzhou, China, 2Sun Yat-Sen University Cancer Center, Guangzhou, China, 3GE Healthcare, Beijing, China
Synopsis
MUSE provides significantly better image quality in CC compared with C-DWI, with no significant difference in ADC.
剧情简介
A recent technology, multiplexed sensitivity encoding (MUSE) diffusion weighted imaging (DWI), was proposed and attracted increasing attention of researchers and radiologists. This approach, which is a multi-shot segmented echo planar imaging (EPI) technique, expands on existing sensitivity encoding techniques by acquiring k-space with an interleaved trajectory with the aim of achieving better spatial resolution and high signal-to-noise ratio (SNR) without the need for navigator pulses between interleaves. In this study, a total of 117 patient with cervical carcinoma (CC) were applied, and our results demonstrated that MUSE provides significantly better image quality in patients with CC compared with conventional DWI (C-DWI), and moreover, the apparent diffusion coefficient (ADC) values obtained by MUSE performed a better diagnostic efficacy for distinguishing squamous cell carcinoma (SCC) and adenocarcinoma (AC), without a significant difference compared with C-DWI.导言
MRI has been widely used in the clinic to preoperatively evaluate CC, with the advantages of allowing for direct visualization of the tumor and having no radiation. DWI could provide not only anatomic and structural information but also quantitative metrics that reflect pathological and physiological conditions of tissues, thus assist in early diagnosis, differential diagnosis and tumor staging. However, based on single shot k-space trajectory EPI, C-DWI are usually unsatisfactory due to the susceptibility artifacts of the tissues caused by blurring from T2* signal decay, particularly at high field strengths and in high resolution imaging. MUSE is a multiplexed DWI reconstruction method in which low-resolution phase from each shot is determined with a sensitivity encoding reconstruction without using extra navigator data. Herein, our study aimed to determine whether MUSE have more advantages than C-DWI in the evaluation of CC.方法
All of the examinations were performed using a 3.0 T whole body scanner (Signa Premier, GE Healthcare) with a digital surrounding body coil. The C-DWI and MUSE sequences were added to the routine clinical MR examination using transverse before administration of contrast agent, and the main scanning parameters were: TR = 3200 ms, TE = minimum, slice thickness = 5 mm, spacing = 1 mm, No. of slices = 30, FOV = 360 × 288 mm, image matrix = 128 * 128 (C-DWI)/160 * 192 (MUES), b value = 50 & 800 s/mm2, No. of excitation = 6 (b = 800 s/mm2), acquisition time = 1 min 22 sec (C-DWI)/2 min 34 sec (MUSE). The overall image quality, geometric distortion, and lesion conspicuity were assessed based on a 5-point Likert scale. Regions of interests (ROIs) were placed on the cervical tumors and the gluteus muscles, and signal to noise ratio (SNR), contrast to noise ratio (CNR) and ADC values were quantified on both sequences. Qualitative scores were compared using Wilcoxon signed-rank test and quantitative parameters were compared using paired t test or Wilcoxon signed-rank test. The mean ADC values were compared using independent t-test for distinguishing SCC from AC. Receiver operating characteristic curve (ROC) analysis was performed to calculate the diagnostic efficacy, and Delong test was used to compare the two ROCs. A value of two-tailed P < 0.05 considered to indicate a significant difference.结果和讨论
MUSE demonstrated better image quality than C-DWI for overall image quality (4.11 vs. 3.20, p < 0.001), geometric distortion (4.08 vs. 3.01, p < 0.001) and lesion conspicuity (4.39 vs. 3.16, p < 0.001). The SNR, CNR of MUSE were significant higher than those of C-DWI (1116.81 ± 583.49 vs. 749.64 ± 414.66, 17.50 ± 7.27 vs. 12.98 ± 5.90, all p < 0.001), with no significant difference in ADC values (936.62 ± 134.81 vs. 923.03 ± 121.22, p = 0.523). The mean ADC value of SCC was significantly lower than that of AC with the area under the curve (AUC) of 0.893 and 0.842 for MUSE and C-DWI (C-DWI: 895.20 ± 104.19 vs. 1050.24 ± 113.80; MUSE: 900.32 ± 108.42 vs. 1102.56 ± 119.71, all p < 0.001), and there was no significant difference between the two ROCs (p = 0.105)(Fig.2).High spatial resolution imaging is important in the assessment of CC as a clear and undistorted tumor delineation, allowing confident diagnosis and accurate evaluation of the local disease extent. However, peristalsis and air in the gastrointestinal tract and vagina exaggerate the artifacts and the geometric distortion on C-DWI, particularly at high field strengths and in high resolution imaging. As a high-resolution DWI technique, MUSE could decrease partial volume effects between lesions and normal structures to reflect truer ADC value.
结论
MUSE provides significantly better image quality in patients with CC compared with C-DWI, with no significant difference in ADC. Furthermore, the ADC value obtained by MUSE performed a better diagnostic efficacy for SCC and AC of CC.Acknowledgements
The authors acknowledge all of the colleagues and participants in Sun Yat-sen University Cancer Center for their support.References
[1] Chen NK, Guidon A, Chang HC, et al. A robust multi-shot scan strategy for high-resolution diffusion weighted MRI enabled by multiplexed sensitivity-encoding (MUSE). Neuroimage. 2013 May 15;72:41-7.[2] Kuang F, Ren J, Zhong Q, et al. The value of apparent diffusion coefficient in the assessment of cervical cancer. Eur Radiol. 2013 Apr;23(4):1050-8.
[3] Patterson DM, Padhani AR, Collins DJ. Technology insight: water diffusion MRI--a potential new biomarker of response to cancer therapy. Nat Clin Pract Oncol. 2008 Apr;5(4):220-33.
[4] Li L, Wang L, Deng M, et al. Feasibility Study of 3-T DWI of the Prostate: Readout-Segmented Versus Single-Shot Echo-Planar Imaging. AJR Am J Roentgenol. 2015 Jul;205(1):70-6.
Figures
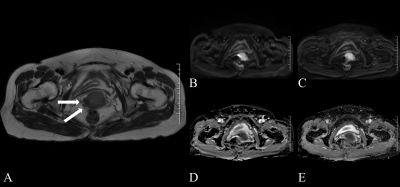
Figure 1. A 50 years old woman with cervical carcinoma. (A) The lesion was shown using white arrows in the T2 weighted image; (B) and (C) C-DWI and MUSE (b value = 800 sec/mm2 ); (D) and (E) ADC maps obtained by C-DWI and MUSE.
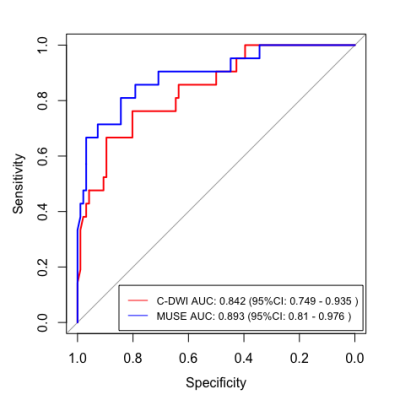
Figure 2. Receiver operating characteristic curves showing the diagnostic performance of the ADC values obtained by C-DWI and MUSE in detecting squamous cell carcinoma and adenocarcinoma.
DOI: https://doi.org/10.58530/2022/2834