2829
Feasibility of T1-weighted USPIO-enhanced MR imaging of pelvic lymph nodes using stack-of-spirals UTE1Medical Imaging, Radboudumc, Nijmegen, Netherlands, 2Comprehensive Pneumology Center, German Center for Lung Research (DZL), Munich, Germany, 3Antaros Medical AB, Mölndal, Sweden, 4Department of Radiology, University Hospital, LMU Munich, Munich, Germany, 5MR Application Predevelopment, Siemens Healthcare GmbH, Erlangen, Germany
Synopsis
Detection of lymph node (LN) metastases can be improved using Ferumoxtran-10, an ultrasmall superparamagnetic particles of iron oxide (USPIO) contrast agent . Commonly, T2* contrast is used to distinguish between normal LNs (high USPIO uptake, low signal) and metastases (low uptake, high signal). T1-weighted imaging may offer complementary information, but is challenging because of the strong T2* effects of the contrast agent. This work investigates whether ultrashort echotime (UTE) imaging with a stack-of-spirals sequence can mitigate this issue. High-resolution USPIO-enhanced T1-weighted UTE of the pelvis was achieved, and T1-mediated signal hyperintensities were indeed observed in LNs in patients with prostate cancer.
Introduction
Detection of pelvic lymph node (LN) metastases can be improved using the ultrasmall superparamagnetic particles of iron oxide (USPIO) contrast agent Ferumoxtran-101. The contrast agent accumulates in healthy lymph nodes through uptake by cells of the immune system, while in metastatic LNs particle accumulation is much lower. USPIO-enhanced MRI for detection of LN metastases is usually based on T2*-weighted (T2*w) imaging, in which LNs with high USPIO uptake exhibit signal loss while LNs with low uptake retain a high signal intensity. T1-weighted imaging may offer complementary information to T2*-weighted imaging in this context, as the R1 and R2* relaxivities of Ferumoxtran-10 differ in their dependency on the microscopic distribution of the USPIO nanoparticles2. Thus, T1w imaging may potentially aid in improving the specificity of USPIO enhanced LN diagnostics. However, obtaining unambiguous USPIO-enhanced T1 contrast is challenging using conventional echo-type sequences, because of the strong T2* effect of the contrast agent. Ultrashort echo time (UTE)-type sequences may mitigate this issue by minimizing T2* relaxation effects. Before any additional value of T1w UTE for LN diagnostics can be investigated, the feasibility of obtaining the desired contrast at sufficiently high resolution3 and image quality must be established. Therefore, the purpose of this study was to assess whether T1-mediated signal enhancement due to USPIO uptake can be observed in pelvic lymph nodes in prostate cancer patients at high isotropic spatial resolution using a stack-of-spirals UTE sequence.Methods
All measurements were performed on a 3T system (MAGNETOM PrismaFit, Siemens Healthcare, Erlangen, Germany) with standard body and spine phased array coils. The prototypical UTE sequence used a stack-of-spirals k-space trajectory with non-selective excitation and variable-duration slice encoding to minimize the effect of T2* decay4,5. The acquisition protocol was optimized in 2 healthy male volunteers (age 30 and 44 years) without USPIO infusion, resulting in the following parameters: coronal slab orientation, TR/TE = 4.3/0.05ms, flip angle 15°, FOV 400 mm, matrix 512, 432 spiral interleaves (corresponding to an undersampling factor of 2) with linear reordering, spiral duration 1160 ms, stack of 256 partitions interpolated to 320, acquisition time 8 minutes. The sequence looped over partitions and spiral angles in its inner and outer loops, respectively. Patients with prostate cancer scheduled for USPIO-enhanced MRI as part of their clinical diagnostic workup were enrolled. Stack-of-spirals UTE was added to the end of their clinical examination, which also included a 3D T1-weighted GRE sequence and a 3D T2*-weighted water-selective MEDIC sequence, both at 0.73 mm isotropic resolution. UTE images were reconstructed offline using the L1-ESPIRiT implementation of the BART toolbox6, employing manual coil selection to reduce streaking artifacts originating from structures outside the FOV. Images were assessed on the presence of signal hyperintensity in LNs, and scored on image quality, visibility of LNs and blood vessels, and artifacts on 5-point scales by a radiologist and a physicist in consensus, both with 7 years of experience in USPIO-enhanced pelvic MRI.Results
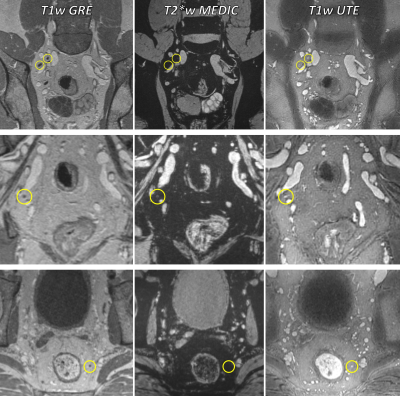
After protocol optimization, four male patients with prostate cancer (age 54-75 years) were included. One of these had had an intraprostatic injection of superparamagnetic iron oxide (SPIO) particles 3 weeks prior to USPIO infusion, and one had surgical clips in the area of interest. Imaging was successful in all 4 patients. Image quality was rated good to excellent in all patients (Figure 1, Table 1), with excellent and strongly hyperintense depiction of the vasculature and high SNR. Although the overall visibility of LNs varied between patients, T1-mediated hyperintensities were observed in at least 1 LN in all patients (Figure 2). Some variations in contrast behavior in T2*-weighted MEDIC and T1-weighted UTE were observed between LNs (Figure 2). Artifacts due to respiratory or bowel motion, streaks, or foldover into the pelvic region were minor (Figure 3). Blooming artifacts were observed in the patients with intraprostatic SPIO injection and surgical clips, but not in the other patients. Chemical shift related artifacts were observed at the borders between watery and lipid tissues (e.g. between muscle and surrounding lipid tissue, Figure 3).Discussion
This work shows that high-resolution T1w USPIO-enhanced MRI of pelvic LNs is feasible in patients with prostate cancer, and that intranodal T1-mediated signal enhancement can indeed be observed. The observed variations in contrast behavior between T2*-weighted and T1-weighted UTE support the hypothesis that T1w imaging may hold complementary information, but larger studies are needed to investigate this further. The fat-water artifact observed at the boundary between muscle and lipid tissue may mimic T1-induced signal enhancement at the boundary between the watery LNs and surrounding lipid tissue. This may be mitigated by using fat suppression techniques, or by decreasing the duration of the spiral readouts. Both would likely lead to an increase in scanning time; however, the high SNR obtained suggests that further acceleration of the acquisition may be possible. Golden angle reordering may then be advantageous for reducing undersampling artifacts.Conclusions
T1-mediated signal hyperintensities can be observed within pelvic LNs of patients post-USPIO infusion using a stack-of-spirals UTE sequence, at 0.8mm isotropic resolution in less than 10 minutes. Although further optimization is warranted, this opens the possibility of investigating the possible additional value of T1w UTE imaging for the diagnosis of LN metastases.Acknowledgements
No acknowledgement found.References
1. Harisinghani MG, Barentsz J, Hahn PF, et al. Noninvasive Detection of Clinically Occult Lymph-Node Metastases in Prostate Cancer. New England Journal of Medicine. 2003;348(25):2491–2499.
2. Brisset J-C, Desestret V, Marcellino S, et al. Quantitative effects of cell internalization of two types of ultrasmall superparamagnetic iron oxide nanoparticles at 4.7 T and 7 T. European Radiology. 2010;20(2):275–285.
3. Fortuin AS, Philips BWJ, Van Der Leest MMG, et al. Magnetic resonance imaging at ultra-high magnetic field strength: An in vivo assessment of number, size and distribution of pelvic lymph nodes. PLOS ONE. 2020;15(7):e0236884.
4. Qian Y, Boada FE. Acquisition-weighted stack of spirals for fast high-resolution three-dimensional ultra-short echo time MR imaging. Magnetic Resonance in Medicine. 2008;60(1):135–145.
5. Mugler III JP, Fielden SW, Meyer CH, et al. Breath-hold UTE Lung Imaging using a Stack-of-Spirals Acquisition. In: Proc. Intl. Soc. Mag. Reson. Med.Vol 23.; 2015:1476.
6. BART Toolbox for Computational Magnetic Resonance Imaging. Available at: DOI:10.5281/zenodo.592960.
Figures
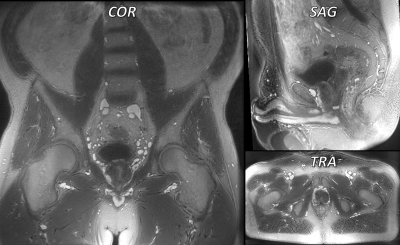
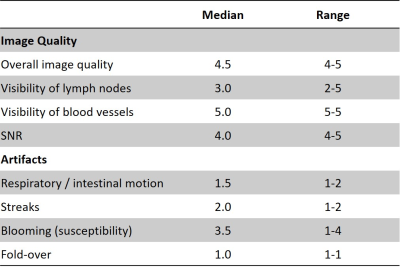
Table 1: Overview of image quality and artifact measures of 4 patients with prostate cancer scanned with T1w USPIO-enhanced stack-of-spirals UTE. Scores for image quality were defined as: 1 - not evaluable; 2 - poor; 3 - moderate; 4 - good; 5 - excellent. Scores for artifacts were defined as: 1 - absent; 2 - minimal; 3 - moderate; 4 - significant; 5 - severe.