2732
Convection triggers local MR signal loss during proton beam irradiation of liquid water phantoms1OncoRay – National Center for Radiation Research in Oncology, Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Helmholtz-Zentrum Dresden-Rossendorf, Dresden, Germany, 2Helmholtz-Zentrum Dresden-Rossendorf, Institute of Radiooncology – OncoRay, Dresden, Germany, 3Department of Radiotherapy and Radiation Oncology, Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany
Synopsis
MRI-based proton beam visualisation in water has proven feasible in exploratory irradiation experiments performed on a first research prototype in-beam MRI system. Beam-induced convection was hypothesised to be implicated into MR signal loss observed within the beam volume. In this study, this hypothesis was tested in liquid water-filled phantoms by suppression of convection-induced motion using mechanical barriers and temperature control of water expansivity. In absence of convection-induced motion, no beam-induced signal changes occurred, supporting the hypothesis that convection triggers local MR signal loss during proton beam irradiation. The elucidation of the exact mechanism of convection-induced signal loss requires further investigation.
Introduction
On-line magnetic resonance imaging (MRI) is expected to improve the targeting accuracy of proton therapy (PT) for moving tumours1. In order to study the interdependence and capabilities of a hybrid system integrating MRI and PT, a low-field open MRI scanner has been integrated with a horizontal fixed proton research beamline at our clinical facility². In first experiments, MRI-based proton beam visualisation has proven feasible in fluid-filled phantoms at high irradiation doses³ allowing image-based localisation of the beam in water. Consequently, this method has been identified as a potential candidate for quality assurance of isocentre alignment of imaging and radiation system components required for accurate treatment planning and dose delivery in MR-integrated PT. It was hypothesised that beam-induced local heating concurrent with a decrease in water density results in upwards-directed convection-induced motion of water molecules, which would in turn lead to the MR signal loss observed within the beam volume³. Experimental testing of this hypothesis, however, was still pending. The aim of this study was therefore to experimentally assess the role of beam-induced convection in MRI-based proton beam visualisation in liquid water phantoms.Methods
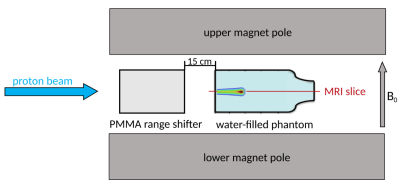
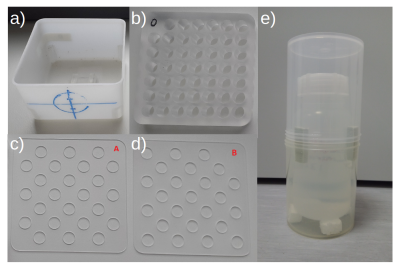
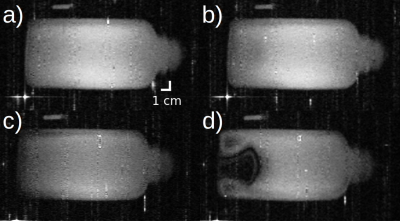
A 0.22 T open MRI scanner (MrJ2200, ASG Superconductors S.p.A., Genoa, Italy) was combined with a fixed proton research beamline². The beam first traversed a range shifter before being stopped within the liquid water-filled phantom positioned centrally in the MRI scanner (Fig. 1). For sequence verification experiments, a cuboid tap water-filled phantom was used (Fig. 2a) which was subsequently supplemented by a capillary insert in combination with horizontal chequerboard patterned flow restriction plates A and B (Fig. 2b-d) to mechanically suppress convection in this phantom4. The capillaries were 15 mm long and had a diameter of 10 mm. An air-insulated tap water-filled flask phantom (Fig. 2e) was used to irradiate the water at a temperature close to 3.98 °C, exploiting the temperature dependence of the volumentric expansion coefficient of water to suppress convection5. Imaging under simultaneous irradiation was repeated after the phantom had assumed the ambient temperature of the scanner overnight. Temperature measurements at both irradiation timepoints were performed in a similar but unirradiated phantom. All phantoms were irradiated for 20 s per image acquisition, irradiation starting 15 s prior to imaging. Proton beam energies between 200 and 215 MeV at beam currents of 8 to 64 nA corresponding to dose rates of 660 to 5100 Gy/min were used. The applied doses ranged from 180 ± 20 to 1400 ± 130 Gy. A gradient echo (GE)-based time-of-flight angiography (TOF-angio) sequence (TE = 7 ms, TR= 19.2 ms, flip angle = 60°, slice thickness = 10 mm, in-plane resolution = 1.18 × 1.07 mm², total scan duration = 3 s) was first tested for its ability to visualise the proton beam assessing its beam energy and current dependence. Subsequently it was used to test the convection hypothesis. The sequence was flow compensated and a 40 mm thick pre-saturation slab was located below the imaging slice, separated by a 10 mm gap. The single-slice images crossed the beam volume horizontally.Results
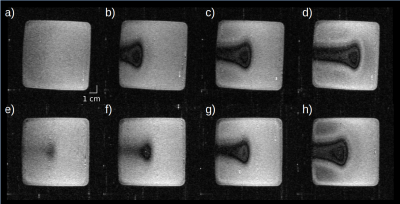
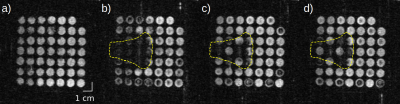
Using the TOF-angio sequence, the stopping proton beam was visualised as a hypointense signature showing partial signal loss within the beam volume in a uniform, free-floating water phantom at room temperature. Moreover, the observed beam signature was found to be beam current and energy dependent (Fig. 3). Mechanical restriction of water mobility using the flow restriction plates to selectively close every second vertical capillary in the water phantom at room temperature resulted in an absence of signal loss within the beam volume in the motion-restricted capillaries, whereas signal loss persisted in the motion-unrestricted capillaries (Fig. 4). Irradiation of free-floating water at 5 ± 1 °C also resulted in an absence of pronounced signal loss within the beam volume compared to irradiation at an ambient temperature of 28 ± 1 °C (Fig. 5).Discussion
The TOF-angio sequence reproduced our previous findings in which beam signatures were visualised as hypointense regions in liquid water through inversion recovery (IR)-GE sequences. The signatures resembled a planar proton dose distribution in shape and showed a clear dependence on beam energy and current3. Consequently, the TOF-angio sequence was found suitable for testing the convection hypothesis. Mechanical as well as thermal suppression of beam-induced convection both resulted in the absence of local upthrust of water molecules responsible for local beam-induced MR signal loss. In the latter case, changes in the mass density of water upon irradiation were prevented exploiting a volumetric thermal expansion coefficient of close to zero at 5 ± 1 °C water temperature.Conclusion
Our experimental results reveal that convection triggers the local MR signal loss observed during proton beam irradiation of liquid water phantoms. Consequently, a translation of this method to humans is unlikely due to the prevailing restriction of convective motion within the narrowly compartmentalised body. For the development of MRI-based geometric quality assurance for hybrid MR-integrated PT systems, the elucidation of the exact mechanism of the convection-induced MR signal loss is the next step to be investigated.Acknowledgements
We thank Julien Smeets and Erik van der Kraaij from Ion Beam Applications S.A. (Louvain-la-Neuve, Belgium) and Andrea Serra from ASG Superconductors S.p.A. (Genoa, Italy) for their support and the fruitful discussions.References
1. Hoffmann A, Oborn B, Moteabbed M, et al. MR-guided proton therapy: a review and a preview. Radiat Oncol. 2020;15:1-13.
2. Schellhammer S, Hoffmann A, Gantz S, et al. Integrating a low-field open MR scanner with a static proton research beam line: proof of concept. Phys Med Biol. 2018;63(23):23LT01.
3. Schellhammer S. Technical feasibility of MR-integrated proton therapy: beam deflection and image quality. Doctoral thesis. Technische Universität Dresden. 2019. https://nbn-resolving.org/urn:nbn:de:bsz:14-qucosa2-341326. Accessed October 25, 2021.
4. Domen S, Krauss A and Roos M. The problem of convection in the water absorbed dose calorimeter. Thermochim acta. 1991;187:225-233.
5. Schulz R and Weinhous M. Convection currents in a water calorimeter. Phys Med Biol. 1985;30(10):1093-1099.
Figures