2670
Application of Fast Field-Cycling (FFC) NMR relaxometry in Colorectal Cancer1Aberdeen Biomedical Imaging Centre, Aberdeen, Scotland, 2Aberdeen Royal Infirmary, Aberdeen, Scotland
Synopsis
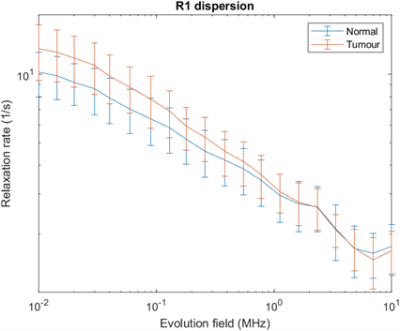
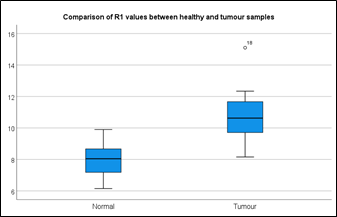
This pilot study was performed to compare healthy and colorectal cancer samples by investigating R1 NMRD profiles acquired with Fast Field-Cycling (FFC) NMR relaxometry. We collected samples from 18 patients and found a significant difference (P=0.001) in the relaxation rates between normal and colorectal cancer tumours below 100 kHz (2.3uT), while this difference became smaller with increasing the magnetic field strengths and disappeared above 1 MHz (23 uT). This dispersion profile may lead to great potential for diagnosis, staging and monitoring treatment response.
The functional alterations induced by pathological processes are commonly viewed clinically as T1-weighted images but are not investigated quantitatively. At the magnetic field strengths used in clinical scanners, changes in endogenous longitudinal relaxation times (T1) do not appear sensitive enough to reflect some tumour characteristics related to tumour stage and aggressiveness1.
Recently, many researchers have investigated the usefulness of ultralow-field magnetic resonance in biomedical applications. Field cycling imaging (FCI) is an emerging technology developed at the University of Aberdeen. It allows changes in the main magnetic field strength during the scan, between 50 μT and 0.2 T 2. This feature can be exploited to observe the field-dependent changes of longitudinal relaxation time (T1), represented as T1 or R1 Nuclear Magnetic Relaxation Dispersion (NMRD) profile, where R1 = 1/T1. This profile provides insights into underlying molecular dynamics information that cannot be accessed by a standard MRI system 3. Previous studies on musculoskeletal and breast cancer found promising biological biomarkers of tumours non-invasively and without the use of contrast media 4,5. This study shows how the relaxation rates differ in colorectal cancer versus normal samples in magnetic fields between 10 kHz and 100 kHz using the FFC-NMR technique.
Methods:
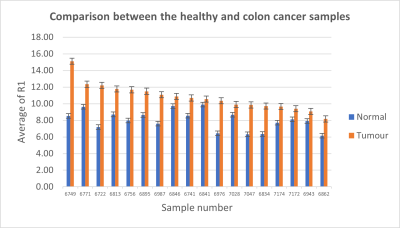
All colorectal tissue samples were obtained via the Grampians Biorepository with the informed consent of the patients. In this pilot study, we obtained 18 fresh resected colorectal tumour samples and corresponding normal counterparts from 18 patients undergoing colorectal cancer surgery (Five Dukes A cases, eight Dukes B cases and Five Dukes C cases). The samples (volume about 1 mL) were measured with a commercial FFC-NMR relaxometer (Stelar S.l.r., Mede, Italy) at a regulated temperature of 37+/-1 °C. The 1H spin-lattice relaxation rate of these samples was investigated between 10 MHz and 700 Hz proton Larmor frequency, using a Field-Cycling pre-polarised and non-polarised pulse sequence.
Statistical tests consisted of a Wilcoxon signed-rank test to compare the relaxation rate (R1) in healthy and tumour samples. All data analyses were conducted using the FitLike software, written in Matlab (version 2021a) and statistics were done using SPSS Statistics 26 (IBM, Armonk, NY, USA) software.
Results:
Experimentation took 20 min per sample. The normality assumption of the data was not met, which motivated the use of the Wilcoxon Signed Ranks Test to determine whether there is a significant difference between normal and tumour samples.
The ex-vivo R1 dispersions showed different profiles between tumour and normal samples; significant differences appeared in the lower field below 100 kHz (Figure 1). Moreover, the average R1 values in tumour samples were significantly higher than the normal samples below 100 kHz (p = 0.001) (Figure 2). This increase in R1 appeared in all the samples (Figure 3).
Discussion:
FFC-NMR measurements were able to discriminate tumours from normal tissues in all 18 cases. This should also be visible in field-cycling imaging, and we have started a study to investigate FFC tumour contrast in vivo on rectal cancer patients.
A previous study has reported that T1 is strongly related to changes in tissue water dynamics within the malignant tissues. The water exchange rate across the plasma membrane is considered a distinctive feature that distinguishes normal from tumour cells6. As shown in our findings, T1 relaxation time is lower in tumour samples. Thus, we suggested that the reported R1 values revealed decreased water volume in the tumour tissues; the suggested reasons are that a specific kind of therapeutic agent causes cell shrinkage, and therefore, reduces the total tissue water7. These processes may lead to decreasing in T1 values and increasing the R1 values. Furthermore, previous studies have indicated that T1 relaxation times are influenced by multiple factors such as vascular and morphologic changes that affect tumour structure and behaviour 6,8. Thus, we think that the NMRD profile has the potential as a new and non-invasive diagnostic biomarker for many pathological conditions to improve diagnosis and patient outcomes.
Conclusion
The herein reported results showed that R1 dispersion profiles, extended to ultra-low fields below 100 kHz, have the potential for the early detection and characterisation of colorectal cancer. Our next project is to demonstrate this finding in vivo and acquire T1-weighted images at different low field strengths using our whole-body 0.2 T FCI scanner.
Acknowledgements
No acknowledgement found.References
1. Johnson, L. M., Turkbey, B., Figg, W. D. & Choyke, P. L. Multiparametric MRI in prostate cancer management. Nat Rev Clin Oncol 11, 346–353 (2014).
2. Broche, L. M., Ross, P. J., Davies, G. R., MacLeod, M.-J. & Lurie, D. J. A whole-body Fast Field-Cycling scanner for clinical molecular imaging studies. Sci Rep 9, (2019).
3. Steele, R. M., Korb, J.-P., Ferrante, G. & Bubici, S. New applications and perspectives of fast field cycling NMR relaxometry. Magnetic Resonance in Chemistry 54, 502–509 (2016).
4. Masiewicz, E. et al. Towards applying NMR relaxometry as a diagnostic tool for bone and soft tissue sarcomas: a pilot study. Scientific Reports 10, 14207 (2020).
5. Broche, L. M. et al. Analysis of musculoskeletal and breast tumours by fast field-cycling MRI. in Abstracts of the 30th Annual Scientific Meeting of the European Society for Magnetic Resonance in Medicine and Biology (ESMRMB). Toulouse, France. October 3-5, 2013 vol. 26 1–150 (Springer Nature Switzerland, 2013).
6. Ruggiero, M. R., Baroni, S., Aime, S. & Crich, S. G. Relaxometric investigations addressing the determination of intracellular water lifetime: a novel tumour biomarker of general applicability. Molecular Physics 117, 968–974 (2019).
7. Yamaguchi, T., Koga, T. & Katsuki, S. Water proton spin-lattice relaxation time during the apoptotic process in ultraviolet-irradiated murine erythroleukemia cells. J Physiol Sci 59, 131–136 (2009).
8. Ravoori, M. K. et al. Tumor T1 Relaxation Time for Assessing Response to Bevacizumab Anti-Angiogenic Therapy in a Mouse Ovarian Cancer Model. PLoS ONE 10, e0131095 (2015).