2586
Readout-segmented Echo-planar Imaging for Determining Cervical Cancer’s Lymph-Vascular Space Invasion and Lymph Node Metastasis Status1Department of Radiology, Affiliated Hospital of Southwest Medical University, Luzhou,SiChuan, China, 2MR Scientific Marketing, Siemens Healthineers, Shanghai, China, 3MR Scientific Marketing, Siemens Healthineers, Xi’an, Shaanxi, China
Synopsis
This study compared the image quality of single-shot echo-planar imaging (ss-EPI) and readout-segmented echo-planar imaging (rs-EPI) in cervical cancer (CC). ADC values derived from these two sequences were considered as diagnostic capabilities for CC’s lymph-vascular space invasion (LVSI) and lymph node metastasis (LNM). The results showed that rs-EPI images of cervical cancer had higher subjective image quality scores, lower SNR, but no difference in CNR and ADC values. ADC was able to predict the CC’s LNM status,but couldn’t identify the LVSI status. ADC of rs-EPI sequence was superior to diagnose CC’s LNM status.
Introduction and Purpose
Lymph-vascular space invasion (LVSI) could predict lymph node metastasis (LNM) and usually be considered as independent prognostic factor for cervical cancer’s recurrence and survival[1]. Due to the existence of functional lymphatic channels around the edge of tumor focus,primary tumor would spread along these marginal areas to regional lymph nodes[2]. Because anterior bladder and posterior gas-containing rectum are challenging regions of anatomy, cervical DWI imaging at 3.0T could easily appear susceptibility artifacts and geometric distortion, especially in these tumor marginal areas. Compared with conventional single-shot echo-planar imaging (ss-EPI) DWI, readout-segmented echo-planar imaging (rs-EPI, known as RESOLVE in Siemens Healthineers) was introduced to improve anatomical accuracy of DWI images by reducing geometric distortion and T2* blurring[3].The purposes of this study was to: (1) compare image quality and ADC values of ss-EPI and rs-EPI DWI in cervical cancer; (2) investigate whether ADC values from ss-EPI or rs-EPI could estimate invasion status of LNM and LVSI in CC patients.
Methods
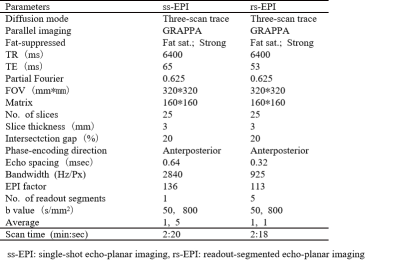
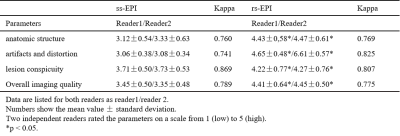
This study included 49 cervical cancer patients who underwent magnetic resonance imaging (MRI) including ss-EPI and rs-EPI DWI before surgery on a 3.0T system (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany). The imaging protocals were listed in Table 1. For each subject, an irregular ROI was manually drawn by two independent radiologists guided by T2WI. ROI included the tumor edge on the biggist image slice,which encompassed the peripheral area within a 5mm radius of the edge of high-intensity tumor and avoided obvious necrotic, higher signal artifacts and deformation areas[4].Regarding to subjective image quality, inter-observer agreement was assessed with Kappa statistics, and qualitative parameters (reader score) between two DWI protocols were compared by using Wilcoxon Signed Rank Test. The quantitative parameters between ss-EPI and rs-EPI were compared by Paired Student's T-Test. Differences in apparent diffusion coefficient (ADC) values were analyzed between (a) CC’s LNM-positive patients’ group (n=9) and LNM-negative (n=40), (b) LVSI-positive (n=20) and LVSI-negative (n=29) by using the Mann-Whitney Test. Diagnostic performances of ADC values were determined by receiver operating characteristic (ROC) analysis.
Result
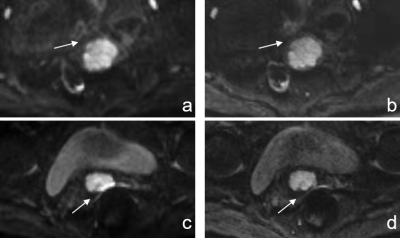
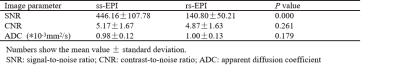
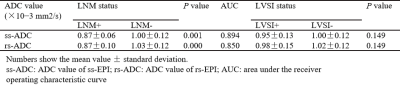
For both observers, rs-EPI achieved significantly better scores in anatomic details, less ghost artifacts and distortion, and overall image quality. The inter-observer agreement between these two independent radiologists was good or excellent (all > 0.75, Table 2). Figure 1 showed the image examples from two patients. SNR values of rs-EPI were lower than those of ss-EPI DWI. No significant difference was found in CNR, ADC values of tumor marginal areas between these two sequences (Table 3). ADC value of the LNM-positive group were substantially lower than that of the LNM-negative group (P < 0.001). However, ADC values of LVSI-positive and LVSI-negative groups showed no difference (P > 0.05). Area under the ROC curve (AUC) of the rs-ADC and ss-ADC values for distinguishing LNM status were 0.894 and 0.850, respectively (Table 4).Discussion and Conclusion
In this study, we found that SNR of rs-EPI was significantly lower than that of ss-EPI, no difference in CNR. Our rs-EPI imaging only collected 5/8 partial fourier data in k-space to shortern the scan time,which may cause some loss of SNR. In order to make the scanning time of these two sequences equivalent and comparable (2min20s vs 2min18s), we also adjusted it by increasing the ss-EPI's average from 0 to 5.SNR and CNR couldn’t represent all of image quality, so we demonstrated the anatomic details, ghost artifacts, and geometric distortion lesion of cervical cancer DWI based on rs-EPI(RESOLVE) were significantly superior to conventional ss-EPI. In this study, rs-EPI has more clear anatomical details, less artifacts and deformation, and higher lesion conspicuity. Last but not least, we indicated ADC of rs-EPI was as reliable as conventional ss-EPI DWI with benefit of better image quality. The results suggest that rs-ADC and ss-ADC both could be used to differentiate CC’s LNM status, and rs-ADC had a better diagnostic efficacy. However, neithor of these two ADC values could predict the LVSI status.
Acknowledgements
We sincerely thank the participants in this study.References
[1] Pol FJ, Zusterzeel PL, van Ham MA, et al. Satellite lymphovascular space invasion: An independent risk factor in early stage cervical cancer. Gynecol Oncol 2015; 138(3): 579-584.
[2] Nathanson SD. Insights into the mechanisms of lymph node metastasis. Cancer 2003; 98(2): 413-423.
[3] Porter DA, Heidemann RM. High resolution diffusion-weighted imaging using readout-segmented echo-planar imaging, parallel imaging and a two-dimensional navigator-based reacquisition. Magn Reson Med 2009; 62(2): 468-475.
[4]Zhou Y, Liu J, Liu C, et al. Intravoxel incoherent motion diffusion weighted MRI of cervical cancer - correlated with tumor differentiation and perfusion. Magn Reson Imaging 2016;34 (8):1 050–1056.
Figures