2581
Can combined DWI, IVIM and DKI predict prognostic factors and genotypes for patients with breast cancer?1Department of Medical Imaging, the affiliated hospital of Jining medical university, Jining,China, jining, China, 2GE Healthcare, MR Research China, Beijing, China, beijing, China
Synopsis
It is essential to accurately preoperatively predict genotypes and prognostic factors for patients with breast cancer in clinic treatment. Combined diffusion weighted imaging (DWI), Intravoxel incoherent motion (IVIM) and diffusion kurtosis imaging (DKI) were developed to comprehensively assess tumors at the cellular and molecular levels. In this study we aimed to explore whether the combination of these three diffusion techniques can help to comprehensively evaluate breast cancer.
Introduction
Breast cancer is the most common malignant cancer in female [1]. Its therapeutic plan and prognosis was closely related to tumor grade, genotypes and proliferation[2,3]. Diffusion MRI, measuring the diffusion behavior of water molecules, has been widely applied for breast cancer detection. Diffusion-weighted imaging (DWI) is now added in routine clinical examination, helping to detect and characterize breast cancer [2,3]. However, the applied mono-exponential model may produce bias in reflecting water diffusion inside tissue [4]. In comparison, multi-b DWI, also called IVIM, enables to separate diffusion from perfusion with bi-exponential model, which cannot be achieved in DWI. DKI, as another advanced diffusion model, evaluating diffusion away from Gaussian distribution in biologic tissues [5], has demonstrated its strength for discriminating malignancies from benign lesions in the breast. However, no study has combined these three different diffusion techniques in breast cancer diagnosis. Therefore, this study aimed to investigate the feasibility of combined DWI, IVIM and DKI, in discriminating the prognostic factors and genotypes of breast cancer.Materials and Methods
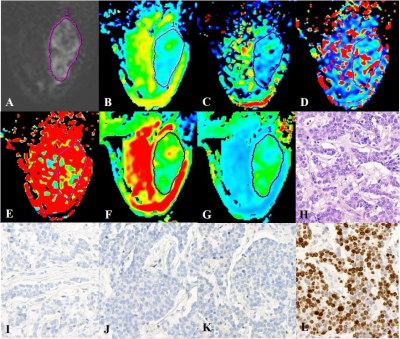
Local Ethics Committee approved the prospective study, and informed consent was obtained from all patients. A total of 229 cases of breast cancer patients confirmed by pathology were collected.The average age was 50.8 ± 10.3 years (range 27–86). All MR scans were performed on an 3T-MRI system (Discovery MR750, GE Medical Systems, USA) with xxx coil employed. DWI, IVIM and DKI were performed in all patients. All DWI, IVIM and DKI data were post-processed using vendor-provided software in GE ADW4.6 workstation. Parametric maps of ADC, true diffusion coefficient (D), perfusion-related diffusion coefficient (D*), perfusion fraction (f), mean diffusion rate (MD) and mean kurtosis value (MK) were obtained accordingly for each patient. The region of interest (ROI) was delineated on the grayscale map with a b-value of 1000 s/mm2, and then, the pseudo-color images of the IVIM and DKI parameters were merged with the grayscale map by using 3D-synchroview (GE Healthcare). The ROI should include as much of the solid region of the tumor as possible, while regions with large blood vessels, cystic changes, and bleeding should be avoided. Pathologic evaluation was performed for the surgically resected specimens by two pathologists (with 4 and 12 years of experience) independently. The prognostic factors include antigen Ki-67 and Nottingham prognostic index (NPI). Clinical identification of different phenotypes is routinely obtained by several molecular markers including estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor (HER-2), and Ki-67 labeling index[7]. All statistic analyses were performed in xxx software. The independent sample t test, Mann-Whitney U test, one-way ANOVA and Kruskal-Wallis H test were used to determine the differences in each parameter among different prognostic factors or phenotypes. Binary logistic regression analyses were used to identify independent factors. Receiver operating characteristic curves (ROC) were used to assess the diagnostic efficacy of each parameter or diffusion model in discriminating prognostic factors or phenotypes, and the Delong test was used to determine whether the area under the ROC curve (AUC) of each parameter was different. P<0.05 was considered statistically significant.Results and discussion
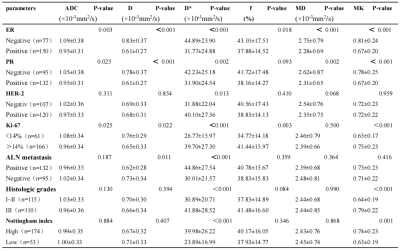
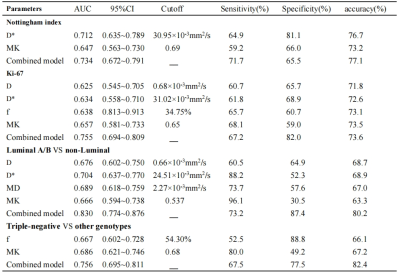
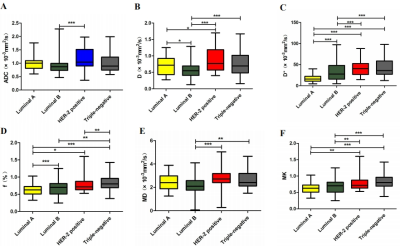
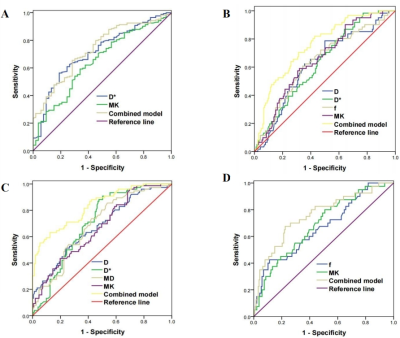
DWI, DKI and DKI derived parameters were compared among different prognostic factors of breast cancer (Table.1, Fig.1). All diffusion parameters were significantly higher in ER negative than ER positive group (P<0.05). Higher ADC, D, D*, MD and MK were shown in PR negative than positive group (P<0.05). For HER-2, only D* was significantly higher in HER-2 positive than negative group (P = 0.013). In addition, D* and MK values were significantly higher in tumors with high-grade (NPI ≥ 3.4) than with low-grade Nottingham group (NPI < 3.4). Significant parameters selected from binary logistic regression analyses were further assessed for diagnostic efficacy using ROC analysis (Table.2,3). For NPI, when D* ≥ 30.95×10-3mm2/s, MK ≥ 0.69, the NPI tended to be high grade, with AUC of 0.712 and 0.647, respectively. The combination of MK and D* showed the highest sensitivity and accuracy of 71.7% and 77.1% (Table.2, Fig.3a). For Ki-67, D*, f and MK were higher and ADC, D values were lower in the high than low Ki-67 expression group (P<0.05). The AUC of the combined model (D+D*+f+MK) was 0.755, being significantly higher than the single parameter (P=0.001~0.006;Table.2, Fig.3b). For molecular subtype groups, Luminal B showed lower D in comparison with other subtypes (P<0.05). D* and f values in Luminal A subtype were significantly lower than other subtypes (P<0.05). Luminal B showed lower MD in comparison with HER-2 positive and Triple-negative subtypes (P<0.05). Both Luminal A and B showed significantly lower MK than HER-2 positive and triple negative types (P<0.05). ROC curves indicated that f≥54.30% and MK ≥ 0.68 cam be significant predictors of Triple-negative subtypes (Fig.3d). Combined f and MK demonstrated superior diagnostic performance with AUC, sensitivity, specificity and accuracy of 0.756, 67.5%, 77.5% and 82.4%, respectively.Conclusion
In conclusion, multiple functional diffusion parameters have demonstrated their potential to identify the genotype and prognosis of breast cancer. The combined DWI, IVIM and DKI models can enhance the diagnostic efficiency, which may contribute to the selection of an appropriate therapeutic approach.Acknowledgements
The author(s) received the following financial support for the research, authorship, and/or publication of this article:Zhejiang Medical and Health Science and Technology Plan Project(202009011151)and Jining Medical and Health key Research and Development Plan Project(2020YXNS012).References
[1] Torre LA, Siegel RL, Ward EM, et al. Global cancer incidence and mortality rates and trends--an update. Cancer Epidemiol Biomarkers Prev, 2016,25:16-27.
[2] Amornsiripanitch N, Nguyen VT, Rahbar H, et al. Diffusion-weighted MRI characteristics associated with prognostic pathological factors and recurrence risk in invasive ER+/HER2- breast cancers. J Magn Reson Imaging. 2018,48:226-236.
[3] Roknsharifi S, Fishman MDC, Agarwal MD, et al. The role of diffusion weighted imaging as supplement to dynamic contrast enhanced breast MRI: Can it help predict malignancy, histologic grade and recurrence?Acad Radiol. 2019,26:923-929.
[4] Dorrius MD, Dijkstra H, Oudkerk M, et al. Effect of b value and pre-admission of contrast on diagnostic accuracy of 1.5-T breast DWI: a systematic review and meta-analysis. Eur Radiol 2014,24:2835-2847.[5] Jensen JH, Helpern JA, Ramani A, et al. Diffusional kurtosis imaging: the quantification of non-Gaussian water diffusion by means of magnetic resonance imaging. Magn Reson Med 2005,53:1432-1440.
[6] Zhang Q, Ouyang H, Ye F, et al. Feasibility of intravoxel incoherent motion diffusion-weighted imaging in distinguishing adenocarcinoma originated from uterine corpus or cervix.Abdom Radiol (NY)2021, 46: 732-744.
[7]Zhang Y, Zhu Y, Zhang K, et al. Invasive ductal breast cancer: preoperative predict Ki-67 index based on radiomics of ADC maps.Radiol Med. 2020,125:109-116.
Figures