2560
Altered Brain Activity and Functional Connectivity between Thalamus and Cortex in Vestibular Migraine: A Resting-State fMRI Study
Xia Zhe1, Yang Huang1, Min Tang1, Kai Ai2, Xiaoyan Lei1, and Xiaoling Zhang1
1Department of MRI, Shaanxi Provincial People’s Hospital, Xi’an, Shaanxi, China, 2Philips Healthcare, Xi’an, China
1Department of MRI, Shaanxi Provincial People’s Hospital, Xi’an, Shaanxi, China, 2Philips Healthcare, Xi’an, China
Synopsis
To investigate the abnormal whole brain functional connectivity patterns in patients with VM by a fully data-driven resting-state functional connectivity methods without any hypothesis. Our findings indicated that whole brain amplitude of low-frequency fluctuation (ALFF) and connectivity abnormalities of these regions may be associated with functional impairments in pain information processing and modulation, transmitting and multisensory integration in patients with VM.
Introduction
Vestibular migraine (VM) is the most common neurological cause of vertigo. 1 Previous studies reported that the thalamus has a pivotal function in nociception as well as in vestibular integration and relay station between the central pain and vestibular systems. It also has been proved to play an important role in cortico-cortical communication through the transthalamic transfer of information between cortical areas that are be involved in vestibular processing. 2 Previous fMRI and PET studies have already confirmed thalamus functional abnormalities in patients with VM. 3-5 However, the key regions involved in the transmission of information changes in the brain function in patients with VM have not been fully elucidated, and findings from previous studies need to be further validated. In order to test the abnormalities in brain activity in the thalamus are related to transmitting information processing in patients with VM, we compared functional connectivity between patients with VM and healthy controls.Methods
Twenty-eight patients with VM and 28 age- and sex- matched healthy controls underwent resting-state functional magnetic resonance imaging (fMRI). Furthermore, the participants completed standardized questionnaires aimed at migraine and vertigo-related clinical features. We examined differences in the ALFF, and brain regions with altered ALFF in the two groups were used as seeds for further whole brain functional connectivity (FC) analysis. Correlation analyses were performed to investigate the relationship between brain dysfunction and clinical features.Results
Compared to the healthy controls, patients with VM showed significantly decreased ALFF in the bilateral thalamus, see Fig 1. A negative correlation was found between ALFF in the left thalamus and the frequency of VM episodes in patients with VM, see Fig 2. Furthermore, patients with VM showed significantly weaker FC between the left thalamus and both regions of the medial prefrontal cortex, and both regions of the anterior cingulum cortex, and the left superior/middle temporal gyrus and the temporal pole, see Fig 3.Discussion
Our study found bilaterally decreased ALFF in the thalamus, indicating a decrease in spontaneous neuronal activity and functional impairment. Furthermore, the decreased ALFF values in the left thalamus were negatively correlated with the frequency of VM attacks. These results suggest that VM might result in weaking of neuronal activity in the thalamus, which is associated with the transmission and processing of pain information. The thalamus plays a critical role in cortico-cortical communication by means of the transthalamic transfer of information between cortical regions.2 Thalamocortical involvement has also been demonstrated in PET studies in VM. 6 In this study, the disruption between the thalamus and these areas may have contributed to abnormal multisensory information integration, pain modulation, and processing in patients with VM.Conclusion
Our results indicated the important role of the thalamus in patients with VM and suggested that connectivity abnormalities of the thalamocortical region contribute to abnormal pain information processing and modulation, transmission and multisensory integration in patients with VM.Acknowledgements
This work was supported by the Social Development Science and Technology Research Project of Shaanxi Province of China (Grant No.2021SF-290).References
1. Formeister EJ, Rizk HG, Kong MA, et al. The Epidemiology of Vestibular Migraine: A Population-based Survey Study [J]. Otol Neurotol, 2018, 39(8): 1037-1044.
2. Sherman SM, and Guillery RW. Distinct functions for direct and transthalamic corticocortical connections [J]. J Neurophysiol , 2011, 106(3), 1068-1077.
3. Russo A, Marcelli V, Esposito F, et al. Abnormal thalamic function in patients Abnormal thalamic function in patients [J]. Neurology, 2014, 82(23), 2120-2126.
4. Teggi R, Colombo B, Rocca, MA, et al. A review of recent literature on functional MRI and personal experience in two cases of definite vestibular migraine [J]. Neurol Sci, 2016, 37(9), 1399-1402.
5. Chen Z, Xiao L, Liu H, et al. Altered thalamo-cortical functional connectivity in patients with vestibular migraine: a resting-state fMRI study [J]. Neuroradiology,2021, Aug 10.
6. Shin JH, Kim YK, Kim H, et al. Altered brain metabolism in vestibular migraine: comparison of interictal and ictal findings [J]. Cephalalgia, 2014, 34(1), 58-67.
Figures
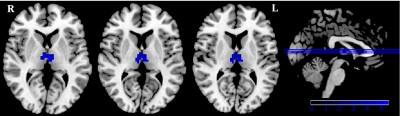
Figure 1. Decreased ALFF in in patients with VM. Two-sample t-test was used to compare the ALFF maps between healthy controls and patients with WM and significantly decreased ALFF in the bilateral thalamus.
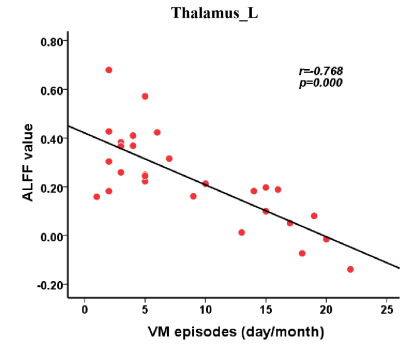
Figure 2. Correlation
analyses between altered ALFF and clinical performances. Significant
correlation between the ALFF of the left thalamus and the frequency of VM
episodes in patients with VM.
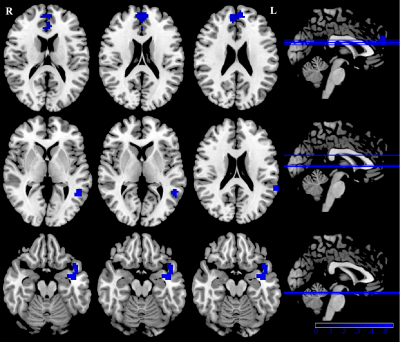
Figure 3. Disrupted
resting-state functional connectivity in patients with VM. Seed based whole
brain resting-state functional connectivities analyses of the bilateral
thalamus was performed, and two-sample t-tests was used to identify disrupted
functional connection between the left thalamus and both regions of the medial
prefrontal cortex, and both regions of the anterior cingulum cortex, and the
left superior/middle temporal gyrus and the temporal pole.
DOI: https://doi.org/10.58530/2022/2560