2507
Reducing streak artefacts in radial MR fingerprinting of the prostate through automated channel removal1Department of Circulation and Medical Imaging, Norwegian University of Science and Technology, Trondheim, Norway, 2Department of Radiology and Nuclear Medicine, St. Olavs hospital, Trondheim University Hospital, Trondheim, Norway, 3Centre for Advanced Imaging, The University of Queensland, Brisbane, Australia
Synopsis
The extreme undersampling factors used in radial magnetic resonance fingerprinting (MRF) of the prostate lead to strong streak artefacts from the femoral arteries and veins. However, it turns out that only a subset of receiver channels is responsible for these streaks. In this work we automatically detected and removed these from the reconstruction pipeline. The method was applied to MRF acquired with various acceleration factors in seven asymptomatic volunteers, significantly reducing visible streaks in reference tissues surrounding the prostate without impairing the prostate T1 and T2 values in the MRF maps.
Introduction
The use of multi-parametric MRI (mp-MRI) has improved the prostate cancer diagnostic pathway [1], but interpretation of the images is still limited by a lack of standardization [2]. Quantitative parameters are ideally independent of the hardware [3], and magnetic resonance fingerprinting (MRF) is a relatively new approach aimed at reproducible quantitative mapping in clinically viable acquisition times [4].One of the key features of the MRF is the use of incoherent undersampling in combination with a model-based reconstruction. For example, a small number of golden angle radial spokes can be used, giving an extreme acceleration factor [5]. However, when applied to the prostate such undersampling tends to lead to streak artefacts from the femoral arteries and veins. Similar artefacts have been reported in traditional radial imaging techniques in the context of bright fat signals, which can be suppressed by removing a subset of receiver channels from the reconstruction [6, 7]. Similarly, we observed that only a small subset of receiver channels is responsible for the inflow related streak artefacts observed in MRF of the prostate. Therefore, we propose a novel method to automatically remove these channels from the data.
Methods
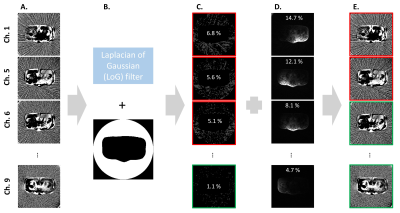
MRF images were acquired with a golden angle radial k-space sampling trajectory [8]. All data was collected on a Magnetom Skyra 3 T MRI system at St. Olavs hospital, Trondheim University Hospital, Norway using a 16-channel body matrix coil in combination with 1-2 channel elements from a table integrated 32-channel spine coil (Siemens, Erlangen, Germany). Pulse sequence design and data post-processing scheme is described in [9], with all data processing done in Matlab (MathWorks, Natick, MA, USA). Seven asymptomatic volunteers (median age: 28, range: 26 – 65 years) were imaged using two spokes (resolution matrix 160x160, field of view 240x240 mm, slice thickness 5 mm and 8 to 10 slices). Two volunteers had additional scans with four and eight spokes, with acquisition times 2:24, 4:49 and 9:37 minutes respectively for 8 slices. The Regional Committee for Medical and Health Research Ethics (REC Central Norway) approved the study, and all volunteers signed informed consents prior to recruitment (REC identifier 2014/1289 and #218665).Channels producing strong streak artefacts were automatically detected in slice five of the complex-valued channel receive sensitivity maps (Irx), which are already part of the post-processing scheme (see Fig. 1): A Laplacian of Gaussian (LoG) filter was applied to detect streaks in the phase of the Irx. An automatically generated mask excluded the body and outer boundaries of the image to avoid detection of confounding edges. Channel streak ratio was then calculated as ratio of detected streak voxels to total mask voxels. The signal contribution of each channel to the final image was estimated using the amplitude of the Irx. Channels with a streak ratio above 1.5 % were removed from all slices, provided that 70 % of the total signal was retained.
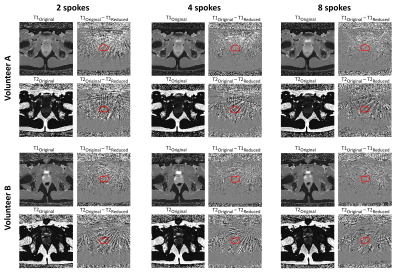
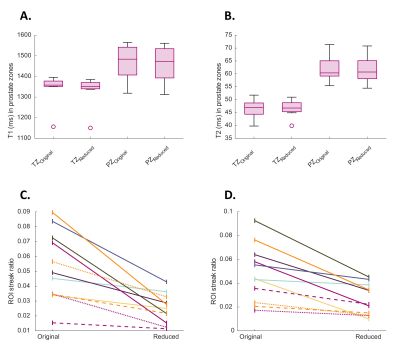
The T1 and T2 values in the prostate before and after channel reduction were compared using expert (radiology resident, E.S.) manual segmentations of the whole prostate gland (WP), peripheral zone (PZ) and remaining zones (named TZ). As the prostate is considered heterogeneous, streak artefact reduction was quantitatively evaluated in the femoral heads and obturator internus muscles surrounding the prostate on the T2 maps. Regions of interest (ROI) were manually drawn and an LoG edge filter was applied to calculate streak ratios (Fig. 2).
Results
The proposed method visibly reduced streak artefacts in two spokes MRF maps (Fig. 3). However, it should be noted that our channel reduction created large variations in the signal sensitivity adding bias to the relative proton density maps. Streak artefacts are less apparent when lower undersampling factors are used, i. e. four or eight spokes, but are reduced even further with the aid of channel reduction (Fig. 4). Importantly, reducing channels has little impact on prostate T1 and T2 values (Fig. 5A and 5B), while reducing the streak ratios in the femoral heads and muscle surrounding the prostate (Fig. 5C and 5D).Discussion
Channel reduction is a simple and fast approach to reduce streak artefacts due to inflow effects from the femoral arteries. However, it does imply sacrifices to the signal to noise ratio (SNR). Some segments of our MRF sequence are expected to be more sensitive to streak artefacts. Only removing signal from streak sensitive segments for selected channels could reduce streaks while maintaining higher SNR, but requires substantial modifications of the dictionary matching process.The total number of receiver channels used varied with subject body size and placement in the scanner. It may be possible to optimize this number to further optimize the trade-off between streak artefact and SNR.
Only one slice was used to detect channels with strong streaks. In the current implementation, detecting and removing channels on a per slice basis will lead to proportional increases in post-processing time. However, this can be addressed using more optimized code.
Conclusion
Removing a strategically chosen subset of receiver channels is a simple yet effective approach to reduce streaks in MRF maps of the prostate without significantly increasing acquisition or post-processing time. Removing streak artefacts while maintaining a high SNR is subject for further research.Acknowledgements
No acknowledgement found.References
1. Lomas, D. J. & Ahmed, H. U. All change in the prostate cancer diagnostic pathway. Nature Reviews Clinical Oncology. 2020;17(6):372–381.
2. Hoang Dinh, A. et al. Characterization of prostate cancer using T2 mapping at 3T: A multi- scanner study. Diagnostic and Interventional Imaging. 2015;96(4):365–372.
3. Mai, J. et al. T2 Mapping in Prostate Cancer. Investigative Radiology 2019;54(3):146–152.
4. Ma, D. et al. Magnetic resonance fingerprinting. Nature, 2013;495(7440):187–192.
5. Cloos, M. A. et al. Multiparametric imaging with heterogeneous radiofrequency fields. Nature Communications. 2016;7(1):12445.
6. Xue, Y. et al. Automatic coil selection for streak artifact reduction in radial MRI. Magnetic Resonance in Medicine. 2012;67(2):470–476.
7. Holme, H. C. M. & Frahm, J. Sinogram-based coil selection for streak artifact reduction in undersampled radial real-time magnetic resonance imaging. Quantitative Imaging in Medicine and Surgery. 2016;6(5):552–556.
8. Winkelmann, S., Schaeffter, T., Koehler, T., Eggers, H. & Doessel, O. An optimal radial pro-file order based on the Golden Ratio for time-resolved MRI. IEEE transactions on medical imaging. 2007;26(1):68–76.
9. Cloos, M. A. et al. Rapid Radial T1 and T2 Mapping of the Hip Articular Cartilage With Magnetic Resonance Fingerprinting. Journal of Magnetic Resonance Imaging. 2019;50(3):810–815.
Figures