2503
Cost-Effectiveness Analysis of Diagnosis of Necrosis from Recurrent Tumor after RT with MRS, MRP and Combined Imaging Method for Low-Grade Glioma1Center for Clinical Spectroscopy, Brigham and Women's Hospital, Boston, MA, United States, 2Radiology, Brigham and Women's Hospital, Boston, MA, United States, 3Radiology, NYU Langone Medical Center, New York, NY, United States
Synopsis
Our decision-analytic model examined the cost-effectiveness of MR Spectroscopy (MRS), MR perfusion (MRP), and the combination of MRS, MRP and DWI for differentiating brain radiation necrosis from tumor progression in high-risk low-grade glioma. Our results suggested that performing combined imaging method had good diagnostic accuracy for a 3-year time horizon but not a cost-effective in the long run. In contrast, MRS and especially MRP alone were more cost-effective over all time horizons. MRS is the most cost-effective method in lifetime when its negative predictive value≥88% at the Willingness-to-Pay threshold of $100,000.
INTRODUCTION
MR Spectroscopy (MRS), MR perfusion (MPR), and the combination of MRS, MRP and DWI are commonly used for differentiating brain radiation necrosis from tumor progression, with sensitivity/specificity as 82%/79%, 83%/86%, and 97%/93%, respectively1. However, the cost-effectiveness of each method remains unknown, especially in the high-risk low-grade gliomas (40 y old or subtotally resected) where long-term treatment and follow-ups are needed2. The objective of this study was to determine the cost-effectiveness of MRS, MRP and the combined imaging method for the differentiation of necrosis from recurrent glioma utilizing a decision-analytic model.METHODS
Model: A decision-analytic model was constructed using a combined decision tree and Markov models based on a published cost-effectiveness analysis of radiation for high-risk low-grade glioma2 (Fig. 1). The goal of the model was to compare cost and effectiveness of three imaging methods: 1) MR Spectroscopy only 2) MR Perfusion only 3) Combined imaging method on the diagnosis of brain radiation necrosis after radiation therapy1. Analysis was performed from a U.S. health system perspective over 3-years, 5-years, 10-years, and lifetime horizons. Input data were derived from systematic literature searches, meta-analyses, cost-effectiveness analysis, and published medical fees (Tables 1&2)1-3. The primary outcome measure in this analysis was the incremental cost-effectiveness ratio (ICER) calculated based on the long-term outcomes in all methods. The effectiveness was measured in terms of quality adjusted life months (QALMs), which was the product of survival rates and the utility associated with a health state. The estimates of QALMs and costs were already discounted at a 3% rate4 from which they were derived to reflect the fact that society prefers to receive benefits sooner rather than later and pay costs later rather than sooner.Sensitivity Analysis: One-way sensitivity analysis was performed on all study variables over a plausible range of values shown in Table 1&2 to recalculate model results to account for variability in factors such as test cost and local expertise. Parameters were assumed to be unrelated to each other. The decision-analytic model and all analysis were performed by using TreeAge Pro 2021 software.
RESULTS
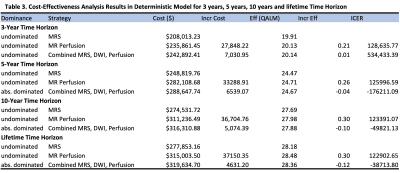
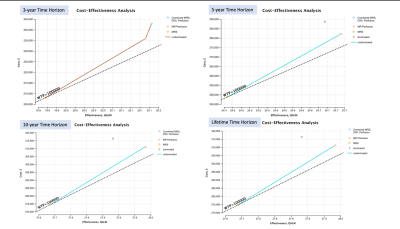
The cost, QALMs and ICERs of the three methods in a deterministic model (Cost-effectiveness-Analysis in Baseline-Case) over 3-year, 5-year, 10-year and lifetime horizons are shown in Table 3. The results showed that there was no dominant method (cost more and less effective) over the 3-year time horizon (Table 3 and Fig 2). However, the combined imaging method costs more and was less effective than MRP-only with lower QALMs and thus the least favored option in 5-year, 10-year and lifetime horizons.At the Willingness-to-Pay (WTP) threshold of $100,000 (Fig 2), MRS was the only method on the threshold line that was favorable method if cost was the only considered factor. However, MRS was the least effective among all methods over all different time horizons (Table 3 and Fig 2). To determine the minimum requirement needed to make MRS a more effective method, we used a one-way sensitivity analysis to test the minimum negative predictive value needed for MRS to diagnose necrosis.
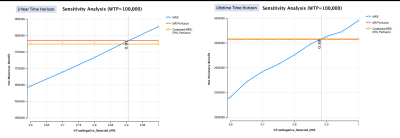
The one-way analysis showed that it required the minimum percent of true negative MRS detected (or its minimum negative predictive value) to be 91% and 88% to make the net monetary benefit of MRS higher than the other two methods over the 3-year and lifetime time horizon, respectively, at a WTP threshold of $100,000 (Fig 3).
DISCUSSION/CONCLUSION
Our results suggest that even though the combined imaging method gave the highest sensitivity and specificity in the current systematic review1, it is effective within the 3-year time horizon but not the most cost-effective option in the long run for the diagnosis of brain radiation necrosis for high-risk low-grade glioma. In contrast, both undominated methods, MRP-only and MRS-only, cost less in the long run, especially MRP-only which showed similar higher effectiveness when compared to the combined imaging method but cost less.MRS was the least expensive method over all time horizons but also the least effective. However, if its negative predictive value≥88%, it could be the most cost-effective method among all at the WTP threshold of $100,000 for lifetime horizon. The drawback of the MR spectroscopy data extracted from Furuse’s systematic review was that the pooled sensitivity and specificity1 were from studies using different MR spectroscopy techniques (including both single voxel and multi-voxel) and different biomarker ratios (including Cho/Cr and Cho/NAA). These differences likely impacted the estimations of long-term cost and effectiveness.
Further research to account for these differences on the MRS technique and other differences from glioma types, long-term treatment options, and their effects are needed to further validate the accuracy and reliability of our model. However, this model was a valuable instrument for assessing the uncertainties and gaps in knowledge in the currently available literature and can serve as a reference point for assessing the studies that should be conducted to improve this model-based approach.
Acknowledgements
No acknowledgement found.References
1. Furuse M., Nonoguchi N., Yamada K., et al., Radiological diagnosis of brain radiationnecrosis after cranial irradiation for brain tumor: a systematic review. Radiation Oncology. 2019; 14:28
2. Qian Y., Maruyama S., Kim H., et al., Cost-effectiveness of radiation and chemotherapy for high-risk low-grade glioma, Neuro-Oncology. 2017; 19(12), 1651-1660.
3. Medical Fees 2018. Practice Management Information Corporation (PMIC) 2018.
4. Kang SK, Hoffman D, Ferket B, Kim MI, Braithwaite RS. Risk-stratified versus Non–Risk-stratified Diagnostic Testing for Management of Suspected Acute Biliary Obstruction: Comparative Effectiveness, Costs, and the Role of MR Cholangiopancreatography. Radiology. 2017;284(2):468-481. doi:10.1148/radiol.2017161714
Figures
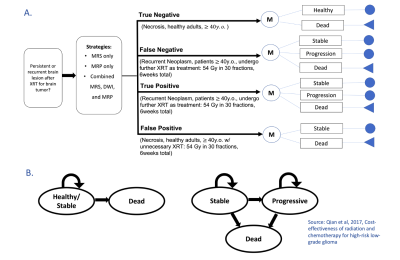
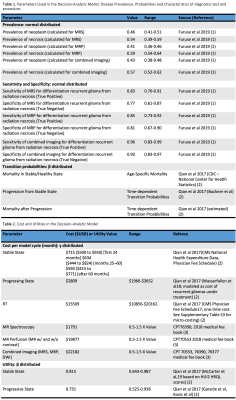
Table 1. Parameters used in the decision-analytic model: disease, prevalence, transition probabilities and characteristics of diagnostic tests.
Table 2. Cost and utilities in the decision-analytic model