2405
Using MRI to Differentiate Synovial Reponses in Patients with Total Knee Arthroplasty
Matthew F. Koff1, Elexis Padgett2, David Landy2, Peter Sculco3, Thomas Sculco3, Timothy Wright2, and Hollis G. Potter1
1Department of Radiology and Imaging, Hospital for Special Surgery, New York, NY, United States, 2Department of Biomechanics, Hospital for Special Surgery, New York, NY, United States, 3Department of Orthopaedic Surgery, Hospital for Special Surgery, New York, NY, United States
1Department of Radiology and Imaging, Hospital for Special Surgery, New York, NY, United States, 2Department of Biomechanics, Hospital for Special Surgery, New York, NY, United States, 3Department of Orthopaedic Surgery, Hospital for Special Surgery, New York, NY, United States
Synopsis
Many patients are satisfied following total knee arthroplasty (TKA) surgery, but post-operative challenges occur. This study evaluated synovial reactions in patients with TKA and related pre-operative MRI findings to direct evaluation of retrieved tibial polyethylene liners from revision surgery. Patients with synovial response of 'arthrofibrosis' had less damage to the tibial insert than patients with a synovial response of 'polymeric'. MRI was able to distinguish specific synovial responses directly to clinically confirmed arthrofibrosis and aseptic loosening.
Introduction
Over 680,000 total knee arthroplasty (TKA) procedures were performed in the US in 2016 alone (1) and this number is expected to increase dramatically over time (2). Most patients are satisfied with the functional outcome of the TKA (3), but many patients subsequently develop arthrofibrosis (4), manifesting as reduced range of motion due to the presence of excessive scar tissue. Standard radiography and computed tomographic imaging are commonly used for post-operative assessment of arthrofibrosis, but lack the inherent soft tissue contrast necessary to visualize the presence and extent of scar tissue. Magnetic resonance imaging (MRI) is a non-invasive, multi-planar imaging modality that utilizes non-ionizing radiation to image tissues adjacent to arthroplasty (5). MRI following arthroplasty is challenging due to significant in-plane and through-plane image distortion, but newer 3D multi-spectral imaging (MSI) techniques mitigate these artifacts to allow detection of bone and soft tissue detail around metallic implants (6,7). MRI has been used successfully to evaluate synovial reactions in TKA patients (8) and gross appearance of the polyethylene tibial insert (9), but a direct comparison to damage of the tibial insert has not been performed to date. Therefore, the purpose of this study was to validate the association of pre-operative synovial reactions assessed by MRI with direct assessment of implant damage on components retrieved from patients undergoing revision surgery.Methods
Patients undergoing revision TKA for stiffness were enrolled in a prospective cohort study along with controls undergoing revision for aseptic loosening or instability. This study had local IRB approval with informed written consent. All subjects were scanned on 1.5T clinical MR scanners with a dedicated lower-extremity coil (GE Healthcare). 2D-FSE images were acquired in the axial, sagittal and coronal planes (10); coronal 3D MAVRIC-SL and MAVRIC-SL STIR images (6) were also acquired. MR images were evaluated and a primary classification of the synovium was assigned: Arthrofibrosis, Focal Scarring, Infection, Mildly Abnormal, or Polymeric (8). The reader was blinded to revision indication. Following surgery, the retrieved polyethylene inserts were evaluated under 22x microscopic magnification and graded for wear damage using the Hood classification system (11). Scoring was performed by 2 independent examiners blinded to revision indication, and the average scores for regions on the implant surface were added to reach a total damage score for the entire insert. Statistical Analysis: Contingency table analysis was performed to detect differences of distributions between primary synovial classification and revision indication. A one-way ANOVA was performed to detect differences of total damage score among synovial classifications. Post-hoc multiple comparisons between synovial classifications were made using Tukey’s HSD test. Statistical significance was set at p<0.05 (SAS V9.4, Cary, NC)Results
Enrollment and data processing has been completed for 69 subjects (16M/53F, 69±9 y.o.) to date. A significant difference in distribution of MRI synovial classifications was found based on revision indication (p<0.0001, Table 1). Most subjects with the MRI synovial classification of arthrofibrosis (Fig. 1) were revised for the clinical diagnosis of arthrofibrosis or stiffness (84%, 16/19), while most subjects with the MRI synovial classification of polymeric (Fig. 1) were revised for aseptic loosening (89%, 17/19). Subjects with focal scaring on MRI presented uniformly for surgical revision indication. In addition, differences of MRI synovial classification were detected by total damage to the polyethylene liner (p<0.0001, Table 1), with subjects assigned a synovial classification of polymeric having greater damage present as compared to classifications of arthrofibrosis and focal scarring (Fig. 2). Examples of synovial reaction appearance on MRI and corresponding pictures of the retrieved polyethylene tibial liner are shown for a patient with arthrofibrosis synovial reaction and a patient with a polymeric synovial reaction. A patient with arthrofibrosis (Fig.3) had heterogenous thickening of the synovial lining and extensive scarring throughout the joint with limited insert wear present. In contrast, the patient with a polymeric synovial response (Fig.4) displayed frondlike hypertrophied synovium on morphologic images, and the retrieved tibial insert had visible regions of pitting, scratching, and embedded cement debris.Discussion
This study compared an indirect assessment of synovial reactions of revision TKA patients using MRI to a direct assessment of damage of retrieved polyethylene liners from the revision surgery. MRI was capable of distinguishing synovial specific responses directly related to clinically confirmed arthrofibrosis and aseptic loosening. In addition, patients classified as having a polymeric synovial response on MRI were closely associated with significantly greater damage to the tibial polyethylene liner. This finding builds on previous work that found an association of abnormal features of TKA seen on MRI with pathologic abnormalities (9). Further, patients with an MRI synovial classification of focal scarring had a varied distribution of revision indication and wide variability of damage to the polyethylene liner. These findings indicate that the presence of focal scarring on MRI may be non-specific in clinical presentation or damage to the implanted components. Future studies may benefit from inclusion of implant rotational alignment as a cofactor in evaluating outcomes.Acknowledgements
We would like to acknowledge the Marina Kellen French Trust Foundation for their support of this study.References
1. Healthcare Cost and Utilization Project (www.hcup-us.ahrq.gov), 2. Singh JA et al., J Rheumatol 2019; 3. Hawker G et al., JBJS 1998; 4. Cheuy VA et al., J Arthroplasty 2017; 5. Sofka CM et al., CORR 2003; 6. Koch KM et al., Magn Reson Med 2011; 7. Hayter CL et al., AJR 2011; 8. Li AE et al., Radiology 2016; 9. Li A et al., AJR 2016; 10. Murakami AM et al., JBJS Br 2012; 11. Hood RW et al., J Biomed Mater Res 1983Figures
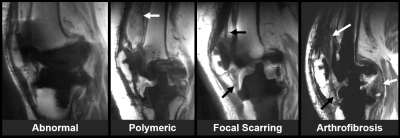
Figure 1. Representative images of
different synovial classifications in subjects with TKA. Arrows indicate
salient features of each categorization in each image.
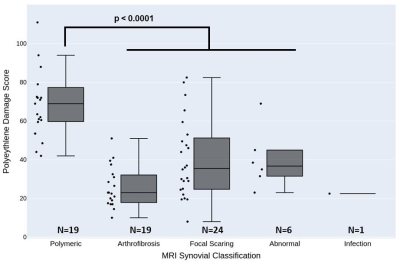
Figure 2. Distribution of damage to
the polyethylene liner for each MRI synovial reaction classification.
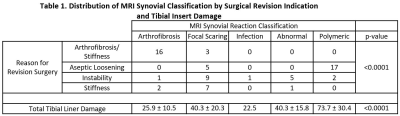
Table 1. Distribution of MRI Synovial
Classification by Surgical Revision Indication
and Tibial Insert Damage
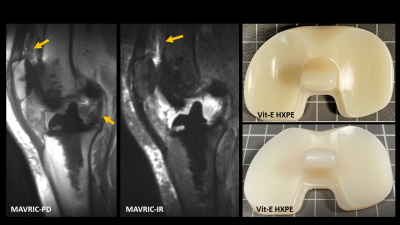
Figure 3. A patient displaying a characteristic
arthrofibrosis response as indicated by the heterogenous thickening of the
synovial lining and extensive scarring throughout the joint. The
retrieved liner displays moderate burnishing and light pitting and scratching
under high microscopy. The implants retrieved for arthrofibrosis had less wear
overall.
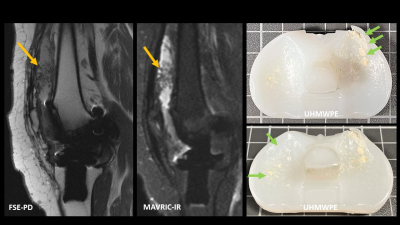
Figure 4. A patient displaying a characteristic
polymeric synovial response as indicated by the frondlike hypertrophied
synovium on both the proton density and inversion recovery images. The retrieved tibial insert has visible
regions of pitting, scratching, and embedded cement debris, causing the
polymeric response observed on MRI due the high likelihood of wear particles
within the joint. Damage was also observed on the post.
DOI: https://doi.org/10.58530/2022/2405