2389
Choroid plexus changes in clinically defined Alzheimer disease spectrum: Volumetry, QSM and BBB permeability imaging1Radiology, Konkuk University Medical Center, Seoul, Korea, Republic of, 2Neurology, Konkuk University Medical Center, Seoul, Korea, Republic of, 3Neurology, Hanyang University Hospital, Seoul, Korea, Republic of, 4Radiology, Chung-Ang University Hospital, Seoul, Korea, Republic of, 5Electrical and Computer Engineering, Seoul National University, Seoul, Korea, Republic of
Synopsis
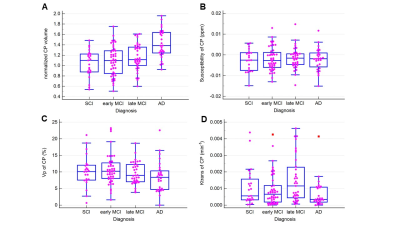
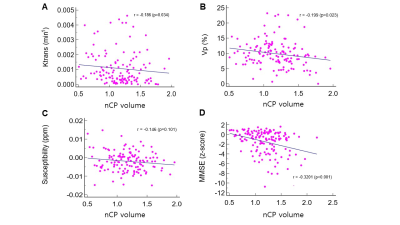
In patients with cognitive impairment spectrum, 3T MRI revealed that choroid plexus volume and permeability was associated with cognitive impairment severity. l In patients with cognitive impairment, choroid plexus (CP) volume followed this order: Alzheimer dementia > late mild cognitive impairment (MCI) > early MCI or subjective cognitive impairment (p<.001) l Large CP volume was associated with lower Ktrans (r=-0.403, p=.006) and Vp (r=-0.543, p=.003) l Increased CP volume was negatively associated with memory function (B=-0.6662, SE=0.2089, p=.002), frontal executive function (B=-0.8973, SE=0.3145, p=.005), and mini-mental status examination score (B=-0.8158, SE=0.3153, p=.01) after adjusting for covariates.
BACKGROUND AND PURPOSE
Mounting evidence indicates that the choroid plexus (CP) plays an important role in the pathophysiology of Alzheimer’s disease (AD), but its imaging profile and its involvement in cognitive impairment are unclear (1,2).Hence, this study aimed to evaluate CP volume and permeability using MRI in patients with cognitive impairments.
METHODS
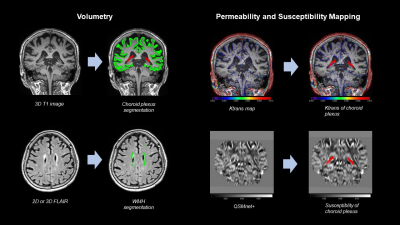
This IRB approved retrospective study collected 532 patients with cognitive complaints who underwent 3T brain MRI between January 2013 and May 2020. The patients consist of a prospective DCE MR cohort (n=132) and retrospective dementia registry (n=400). 3D T1-volume images, 2D or 3D FLAIR images, and 3D susceptiblity-weighted images or 3D multi-dynamic gradient echo images. A coronal 3D DCE sequence (voxel size: 1.25 x 1.25 x 3 mm) was obtained with 60 dynamics and a time resolution of 10 seconds and a standard dose of gadobutrol (Gadovist, Bayer Healthcare, Berlin, Germany). A pre-contrast T1-weighted gradient echo MR sequence (3.10/0.97) was obtained for T1 mapping CP volume was obtained by automatic segmentation (Freesurfer 6.0 platform enhanced with a deep learning algorithm for brain extraction and segmentation)(3) using T1 volume images. The Patlak permeability model was used to generate permeability parameters (Ktrans and Vp) from dynamic contrast-enhanced imaging using NordicICE software (version 4.1.3)(4). QSM images were generated by using QSMnet+ as previously described(5). The effects of the CP volume on cognitive function were evaluated using multivariable regression after adjusting for confounding factors.RESULTS
Evaluated were 532 patients with cognitive complaints (mean age, 72.2 ± 8.59 years; 388 women). Patients with subjective cognitive impairment and early mild cognitive impairment (MCI) were younger than patients with late MCI and AD (p < .001). A significantly higher CP volume was observed in patients at more severe disease stages (p < .001). Lower Ktrans (r = -0.403, p = .006) and Vp (r = -0.543, p = .003) values were associated with a larger CP. An increased CP volume was negatively associated with memory function (B = -0.6662, standard error (SE) = 0.2089, p = .002), frontal executive function (B = -0.8973, SE = 0.3145, p = .005), and Mini-Mental Status Examination z-score (B = -0.8158, SE = 0.3153, p = .01) after adjusting for covariates.DISCUSSION and CONCLUSIONS
Our result suggests a more complex relationship between CP permeability and CP volume. While in this study, CP permeability increased with CP volume in early MCI patients, this CP permeability-volume correlation disappeared in the other subgroups. Changes in CP permeability might show a non-linear relationship with disease severity as those of amyloid deposition in AD.On the other hand, the relationship between Vp and cognitive impairment is more straightforward. The present results suggest that the capillary blood flow of the CP decreases with increasing CP volume in patients with AD.In conclusion, CP volume increased with disease progression in patients with cognitive impairment. Alterations in CP permeability are associated with disease severity. CP volume and permeability may be useful imaging markers for AD-related cognitive impairment, independent of amyloid pathology or neurodegeneration.
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant, funded by the Korean government (MSIP) (grant number 2020R1A2C1102896) and the Korea Health Technology R&D Project through the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number HI21C0222).References
1. van der Kant R, Goldstein LSB, Ossenkoppele R. Amyloid-beta-independent regulators of tau pathology in Alzheimer disease. Nat Rev Neurosci 2020;21(1):21-35. doi: 10.1038/s41583-019-0240-3
2. Serot JM, Bene MC, Foliguet B, Faure GC. Morphological alterations of the choroid plexus in late-onset Alzheimer's disease. Acta Neuropathol 2000;99(2):105-108. doi: 10.1007/pl00007412
3. Lee J, Lee JY, Oh SW, Chung MS, Park JE, Moon Y, Jeon HJ, Moon WJ. Evaluation of Reproducibility of Brain Volumetry between Commercial Software, Inbrain and Established Research Purpose Method, FreeSurfer. J Clin Neurol 2021;17(2):307-316. doi: 10.3988/jcn.2021.17.2.307
4. Moon WJ, Lim C, Ha IH, Kim Y, Moon Y, Kim HJ, Han SH. Hippocampal blood-brain barrier permeability is related to the APOE4 mutation status of elderly individuals without dementia. J Cereb Blood Flow Metab 2021;41(6):1351-1361. doi: 10.1177/0271678X20952012
5. Jung W, Yoon J, Ji S, Choi JY, Kim JM, Nam Y, Kim EY, Lee J. Exploring linearity of deep neural network trained QSM: QSMnet(.). Neuroimage 2020;211:116619. doi: 10.1016/j.neuroimage.2020.116619
Figures