2383
Disrupted brain functional network connectivity in Parkinson’s disease patients with Mild Cognitive Impairment.1Cleveland Clinic Lou Ruvo Center for Brain Health, Las Vegas, NV, United States
Synopsis
The underlying cause of cognitive deficits in PD (PD-MCI) is not well understood and there are no biomarkers to diagnose PD-MCI. Although previous studies have found disrupted functional connectivity several factors make it difficult to generalize findings from fMRI studies. In the current study, we investigate functional network abnormalities in PD-MCI and PD patients who are cognitively normal (PD-NC). Our results were in line with earlier studies that showed altered connectivity was observed involving the frontal and striatal regions in the PD-MCI group, and we also found altered connectivity between regions in the temporal and the parietal cortex.
Introduction
Cognitive deficits are common and affect about 15%-40% of early-stage Parkinson’s disease (PD) patients [1]. Studies have shown that mild cognitive impairment in PD patients (PD-MCI) is a risk factor for the development of dementia over time [2]. However, not all PD-MCI patients progress to dementia and it is still not clear whether there are distinct features that lead to conversion from MCI to dementia in PD patients. The underlying cause of cognitive deficits in PD is not well understood and there are no biomarkers to diagnose PD-MCI [3]. Earlier studies have identified altered functional connectivity involving frontostriatal regions in the PD-MCI group [4], but the different experimental and analytic approaches, disease duration, a priori model and analytic assumptions, and cohort differences make it difficult to generalize findings from fMRI studies [5]. In the current study, we aim to quantify the connectivity differences using high temporal resolution data and a well-characterized group of patients to potentially expand upon prior such investigations that have shown functional connectivity differences between the PD–MCI and PD patients who are cognitively normal (PD-NC).Methods
Resting-state fMRI (rs-fMRI) data were obtained from 47 HC (26 Females; Age: 70.35±6.33years; Years of Education (YOE): 16.37±2.42years) and 27 PD participants. 14 PD participants were identified as PD-NC (5 Females; Age: 68.07±6.99years; YOE: 15.33±2.19years)) and 13 PD participants were identified as PD-MCI (3 Females; Age: 67.64±6.6years; YOE: 15.43±2.6years) A consensus diagnosis of PD-MCI was made by a practicing neurologist and neuropsychologist based on clinical presentation and neuropsychological evaluations of each participant. For diagnostic accuracy, PD-MCI was classified after applying a threshold of 1.5 standard deviations below appropriate norms on at least two neuropsychological tests following Movement Disorders Society (MDS) criteria [1]. All PD participant data used in this study were obtained in the clinically defined ON state. 850 volumes were acquired at a TR of 700 ms on a 3T MRI scanner. After standard preprocessing, time series were obtained from 246 different ROIs identified based on the Brainnetome atlases [6]. The connectivity between two ROIs was estimated using Pearson’s correlation between their time-series, and a 246 x 246 connectivity matrix was obtained for each subject. Network-based statistic (NBS) [7] was used to perform nonparametric statistical tests to identify whether there was a difference in functional connectivity between the different groups (HC vs PD-MCI; HC vs PD-NC; PD-NC vs PD-MCI). Significance was established at p<0.05.Results
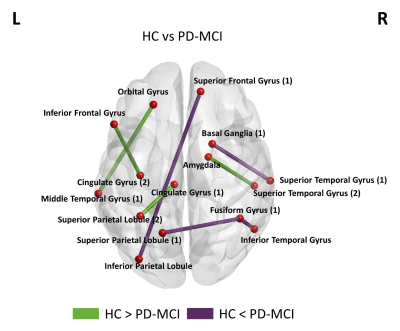
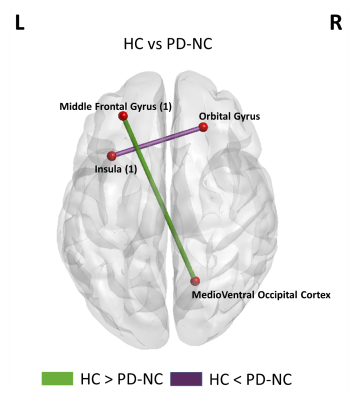
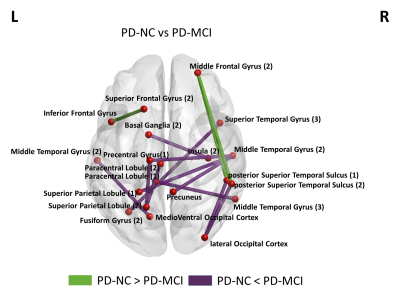
HC vs PD-MCI: Fig.1 shows a set of 8 paths significantly different between the HC group and PD-MCI groups. The PD-MCI group showed reduced connectivity in paths (green color) comprising the amygdala, and regions in the frontal and temporal lobes and increased connectivity in paths (purple) comprising the parietal lobe regions, basal ganglia, and frontal lobe regions compared to the HCs. HC vs PD-MCI: Fig.2 shows the 2 paths significantly different between the HC group and PD-NC groups. The connectivity between the occipital cortex and the middle frontal gyrus was significantly higher and the connectivity between the insula and orbital gyrus was significantly lower in the HC group when compared to the PD-NC group. PD-NC vs PD-MCI: Fig.3 shows a set of 14 paths significantly different between the HC group and PD-MCI groups. When compared to the PD-NC group the PD-MCI group showed reduced connectivity (green color) in only 3 of those paths comprising regions in the temporal and frontal lobes while there was increased connectivity in 11 paths (purple) between several regions in the parietal lobe, occipital lobe, basal ganglia, and insular gyrus. Results were visualized with the BrainNet Viewer (http://www.nitrc.org/projects/bnv/) [8].Discussion
These findings expand upon prior investigations in that 1) altered connectivity was observed involving the frontal and striatal regions in the PD-MCI group, and 2) altered connectivity was also observed between regions in the temporal and the parietal cortex. Within this ongoing study, connectivity differences in the clinically defined OFF state, and correlations with behavioral measures in both ON and OFF states, are underway to better understand the relationship between functional connectivity and cognition and how it is affected by dopaminergic medication.Acknowledgements
This study is supported by the National Institutes of Health (grant 1R01EB014284, R01NS117547, P20GM109025, and P20AG068053), a private grant from the Peter and Angela Dal Pezzo funds, a private grant from Lynn and William Weidner, a private grant from Stacie and Chuck Matthewson and the Keep Memory Alive-Young Investigator Award (Keep Memory Alive Foundation).References
[1] Litvan I, Goldman JG, Tröster AI, et al. Diagnostic criteria for mild cognitive impairment in Parkinson’s disease: Movement Disorder Society Task Force guidelines. Mov Disord. 2012/01/24. 2012;27:349–356.
[2] Hely MA, Reid WG, Adena MA, Halliday GM, Morris JG (2008): The Sydney multicenter study of Parkinson’s disease: The inevitability of dementia at 20 years. Mov Disord 23:837–844.
[3] Goldman JG, Litvan I. Mild cognitive impairment in Parkinson's disease. Minerva Med. 2011;102(6):441-459.
[4] Monchi O, Hanganu A, Bellec P. Markers of cognitive decline in PD: The case for heterogeneity. Parkinsonism Relat Disord. 2016 Mar;24:8-14. doi: 10.1016/j.parkreldis.2016.01.002. Epub 2016 Jan 7. PMID: 26774536.
[5] M. Tahmasian, L.M. Bettray, T. van Eimeren, A. Drzezga, L. Timmermann, C.R. Eickhoff, S.B. Eickhoff, C. Eggers, A systematic review on the applications of resting-state fMRI in Parkinson’s disease: Does dopamine replacement therapy play a role?, Cortex. 73 (2015) 80–105. doi:10.1016/j.cortex.2015.08.005.
[6] Fan L, Li H, Zhuo J, Zhang Y, Wang J, Chen L, Yang Z, Chu C, Xie S, Laird AR, Fox PT, Eickhoff SB, Yu C, Jiang T. The Human Brainnetome Atlas: A New Brain Atlas Based on Connectional Architecture. Cereb Cortex. 2016 Aug;26(8):3508-26. doi: 10.1093/cercor/bhw157. Epub 2016 May 26. PMID: 27230218; PMCID: PMC4961028.
[7] Zalesky A, Fornito A, Bullmore ET. Network-based statistic: identifying differences in brain networks. Neuroimage 2010; 53: 1197–1207.
[8] Xia M, Wang J, He Y (2013) BrainNet Viewer: A Network Visualization Tool for Human Brain Connectomics. PLoS ONE 8(7): e68910. doi:10.1371/journal.pone.0068910.
Figures