2206
Ultrahigh-Field 7T MRI of the Brain of COVID-19 Patients with Neurological Symptoms: An Initial Study1Diagnostic, Molecular and Interventional Radiology, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 2BioMedical Engineering and Imaging Institute, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 3Neurology, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 4General Internal Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Synopsis
Since late 2019, COVID-19 has emerged as a global pandemic that has infected 200 million and killed 5 million. A significant proportion of COVID-19 patients continue to have persistent neurological sequelae after recovery, which are not well understood. In this study, we report our preliminary neuroradiological findings from ultrahigh field MRI at 7T in patients with post-COVID neurological symptoms. We show that numerous heterogeneous abnormalities are present in 7T MR brain images. We expect that these findings may pave the way to explain neurological symptoms in post-COVID patients.
Introduction
Since late 2019, the novel coronavirus disease 2019 (COVID-19), which is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has emerged as a global pandemic1. It is highly contagious, still ongoing and is confirmed to have infected 200 million and killed 5 million people worldwide2. While many COVID-19 patients recover without any notable lasting symptoms, a significant proportion of COVID-19 patients continue to have persistent neurological sequelae3 including stroke, visual defects, anosmia/dysgeusia, brain fog4, among others. To date, these manifestations are not well understood. Long-haul COVID-19 syndrome4 is expected to become a serious healthcare burden in the next several years5. Here, we report our preliminary neuroradiological findings from ultrahigh field MRI at 7T in patients with post-COVID neurological symptoms.Methods
In this study, 8 patients (age: 54 ± 10, 4 female), who had recovered from COVID-19 and presented with post-COVID neurological symptoms, were enrolled. All patients underwent whole brain MRI on a Siemens Magnetom 7T scanner (Siemens Healthineers, Erlangen, Germany) using a 1Tx/32Rx head coil (Nova Medical, Wilmington, MA). The MRI protocol was specifically developed for this COVID-19 study and included axial T1-weighted MP2RAGE, FLAIR, T2-weighted TSE, susceptibility weighted imaging (SWI), as well as coronal-oblique T2-weighted TSE (imaging plane oriented perpendicular to olfactory bulbs) and a T2*-weighted multiecho spoiled-gradient-echo sequence to capture the brainstem perpendicular to the imaging plane (Siemens MEDIC sequence, shimmed across brainstem). (The protocol also included DTI, ASL and rs-fMRI). Images were evaluated by 3 fellowship-trained neuroradiologists for T2/FLAIR hyperintensities (based on the Fazekas scale), infarcts, chronic microhemorrhages and macrohemorrhages, encephalopathy features, brain volume loss (qualitative), olfactory bulb abnormalities and brainstem abnormalities. Findings that differed among the readers were reviewed and adjudicated in consensus.Results
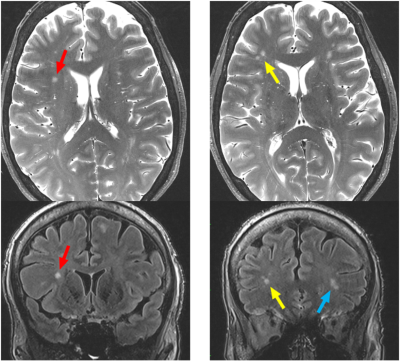
The post-COVID neurological symptoms of each patient are listed in Table 1. The neuroradiological findings from 7T MRI are also listed in Table 1. The neuroradiological findings were heterogeneous across the patients. No infarcts and no encephalopathy features were observed in any patient. Bilateral olfactory bulb thinning (Figure 1) was observed in Patient 4, who presented neurological symptoms of dysgeusia and COVID long haul syndrome. Brainstem abnormalities were observed in two patients: microhemorrhage in the left dorsal pons Patient 2 and hyperintensity in the lower medulla tracts in Patient 4. Figure 2 shows three images of the brainstem in Patient 4 acquired with the multiecho spoiled-gradient-echo sequence (Siemens MEDIC).Chronic microhemorrhage was observed in Patient 3 in the left frontal subinsular region (Figure 3A). Chronic macrohemorrhage was observed in Patient 2 in the right frontal cortex (Figure 3B). Both Patients 2 and 3 presented with the neurological symptom of encephalopathy. Moderate FLAIR/T2 hyperintensities (Fazekas scale 2) were observed in Patient 6 (Figure 4). Patient 6 presented with several neurological symptoms including COVID long haul syndrome, numbness, headache and blurry vision, as listed in Table 1. Mild hyperintensities (Fazekas scale 1) were observed in 6 patients.
The following incidental findings, which are likely unrelated to COVID-19, were observed: arachnoid cysts in two patients and prominent arachnoid granulations in four patients.
The time between COVID-19 diagnosis and 7T MRI was 12 ± 5 months.
Finally, it should be noted that Patients 2, 3 and 4 were hospitalized at the time of COVID-19 infection and underwent brain MRI at 1.5T as part of their clinical care. These acute-stage 1.5T MRI exams did not reveal any abnormalities.
Discussion
In this ongoing study, we report our preliminary neuroradiological findings from brain MRI at 7T in 8 patients with post-COVID neurological symptoms. The neuroradiological findings are very heterogeneous. It is interesting that these findings persist even after 12 months post COVID infection. In particular, three of the patients in this study underwent brain MRI at 1.5T as part of their clinical care during COVID-related hospitalization, and those patients did not present any findings from the 1.5T MRI exams at the acute phase, even though they presented findings from 7T MRI. The reason for this is unknown: it is possible that this is due to the lack of high resolution and SNR in the clinical exams, or that these findings are chronic in nature. It is also interesting that 4 of 8 patients presented the incidental finding of prominent arachnoid granulations. This may indicate lymphatic involvement in the neurotropism of SARS-CoV-2 virus.It should be noted that thinning of the olfactory bulbs was observed in one patient. However, this patient presented dysgeusia as a neurological finding, and not anosmia. Anosmia is more likely to be related to thinning of the olfactory bulbs. It is possible that the patient did have anosmia but failed to report it (both anosmia and dysgeusia are often concurrent in COVID-19).
Because of the small sample size of this study, it was not possible to derive any associations between the neurological symptoms and the 7T neuroradiological findings. We would like to note that this study is ongoing and in the early stages, and we expect to have a larger sample size of both post-COVID patients and age and sex-matched healthy controls very soon. We expect to find meaningful links between 7T neuroradiological findings and neurological symptoms in a larger cohort of post-COVID patients.
Acknowledgements
The authors would like to acknowledge the National Institutes of Health (NIH) for the following sources of funding support for this study:
NIH NINDS 1R21NS122389-01
NIH NCI 5R01CA202911-05
References
1. Chen N, et al., Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet, 2020. 395(10223): p. 507-513.
2. Ritchie H, et al., "Coronavirus Pandemic (COVID-19)", 2020, Published online at OurWorldInData.org. Retrieved from: https://ourworldindata.org/coronavirus on Nov. 2021 [Online Resource]
3. Ladopoulos T, et al., “COVID-19: Neuroimaging Features of a Pandemic”. J Neuroimaging, 2021. 31(2): p. 228-243
4. Asadi-Pooya AA, et al., “Long COVID syndrome-associated brain fog”, J Med Virol. 2021 Oct 21. doi: 10.1002/jmv.27404. (Online ahead of print).
5. Higgins V, et al., “COVID-19: from an acute to chronic disease? Potential long-term health consequences”. Crit Rev Clin Lab Sci. 2021 Aug;58(5):297-310. doi: 10.1080/10408363.2020.1860895. Epub 2020 Dec 21. PMID: 33347790.
Figures
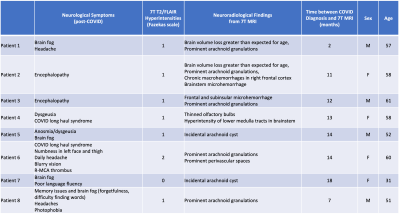
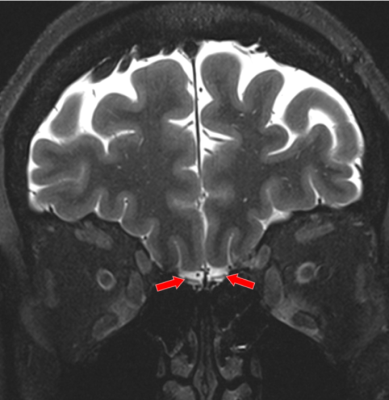
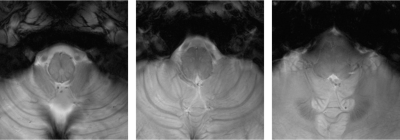
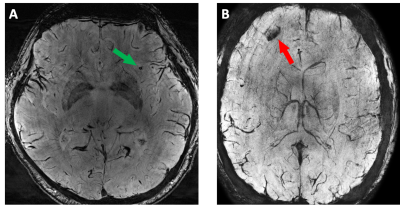
Figure 3: A: Susceptibility in left frontal subinsular region (green arrow) indicating chronic microhemorrhage in Patient 3.
B: Susceptibility in right frontal cortex (red arrow) indicating chronic macrohemorrhage in Patient 4.