2182
Metasurface-based pad for improving fetal imaging at 3T1School of Physics and Engineering, ITMO University, Saint Petersburg, Russian Federation, 2Federal Almazov North-West Medical Research Center, Saint Petersburg, Russian Federation, 3Department of Radiology, C.J. Gorter Center for High‐Field MRI, Leiden University Medical Center, Leiden, Netherlands
Synopsis
Radiofrequency magnetic field homogeneity improvement and SAR reduction are two essential tasks for fetal MRI at 3T. We demonstrate for the first time that the metasurface-based pad can effectively improve the transmit efficiency while reducing SAR within the entire fetus and fetus brain. The metasurface is assembled from the metal wires loaded with capacitors. Numerical studies of a pregnant woman voxel model in the 9th month covered with the proposed metasurface centered within fetus brain (body) showed 25% (28%) transmit efficiency improvement and up to 9% (2.8%) increased magnetic field homogeneity, while the whole-body SAR was reduced by 1.2 (1.6)-fold.
Introduction
The interest of the scientific and medical community in 3T MRI of the fetus continues to grow. Mainly because 3T scanners, in contrast to 1.5T, offer a higher spatial resolution, providing more precise fetal depiction with reduced scan time1. However, at a higher magnetic field strength, radiofrequency (RF) wavelength becomes comparable with the sizes of the body, leading to the constructive and destructive interference of the standing waves2. As a result, local areas of brightening or dark occur, especially at the last months of pregnancy or in females with multiple fetuses. Passive shimming with dielectric pads, consisting of mixed ceramic powders and heavy water, have been introduced to increase the RF magnetic field in low-transmit efficiency regions for abdominal3 and fetal4 imaging. However, the main drawback of the dielectric pads is their weight of up to 2-4 kilograms that significantly affects the patient’s comfort. Recently, an ultralight and compact metasurface to improve abdominal imaging at 3T was proposed5. Here, we study the effect of the optimized metasurface-based pad for a realistic pregnant model and compare its performance with the state-of-the-art dielectric pad.Methods
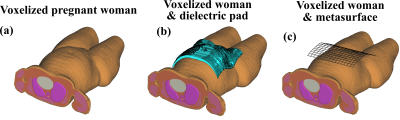
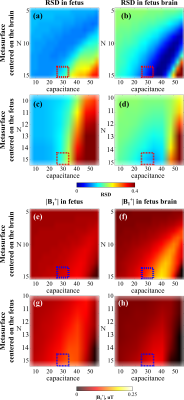
Numerical studies were performed in CST Microwave Studio 2021. A voxel model (BCH3, BMI=28 kg/m2) generated from an MRI of a pregnant woman in the ninth mount was used6. The RF magnetic field (B1+) excitation was carried out using the whole-body birdcage coil tuned to 123 MHz. Three cases were compared: only birdcage coil with a female model, birdcage coil with (2) dielectric pad4 (size = 30×25 cm2, ε = 248), and (3) metasurface (Figure 1). The proposed metasurface consists of a set of metal crosses (2×2 cm2) connected by capacitors. The metasurface was located in two positions: centered on the fetus or the fetal brain. The optimization of the structure was performed using the homogeneous phantom consisting of three parts: the homogeneous body of a woman, the fetus body, and the fetus brain (reconstructed from the voxel model mentioned above). The average values of the B1+ amplitude and the relative standard deviation (RSD) were calculated for different configurations according to the number of metasurface unit cells (N) and the capacitances of capacitors (Figure 2). The most effective case, which provides the highest B1+ amplitude (N=15, cap=40 pF), has a resonance at the operating frequency, leading to additional artifacts in the form of B1+ minima in the phantom volume. Therefore, a compromise metasurface geometry (N=15, cap=30 pF) that works up to the first resonance was chosen (the hatched rectangle in Figure 2a-h). The SAR was evaluated in terms of the whole-body SAR (SARwb) equal to 2 W/kg according to the recommendations of the International Electrotechnical Commission7. The SAR results were normalized to the average B1+ magnitude in the region of interest (ROI), i.e., brain/entire fetus.Results
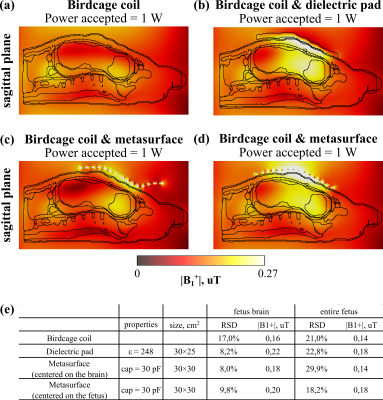
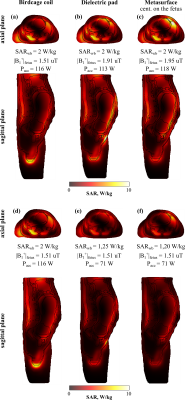
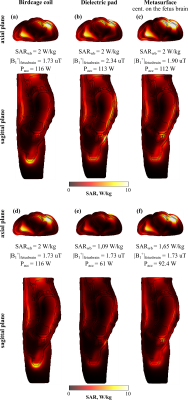
Figure 3 shows simulated B1+ maps for three cases: (1) without any pad, with (2) conventional dielectric pad, and (3) metasurface-based pad centered on the fetus or the fetal brain. One can observe the B1+ inhomogeneity in the ROIs for the reference case (Figure 3a). Adding the dielectric pad and the metasurface-based pad improves the B1+ in ROIs (Figure 3b-d) for almost all cases, which is confirmed by the decrease in RSD for both cases (Figure 3e). The exception is the case for the entire fetus ROI with the dielectric pad; in this case, RSD slightly increased from 21% to 22.8%, while the metasurface-based pad centered on the entire fetus RSD was reduced to 18.2%. At the same time, the transmit efficiency was improved by 1.3-fold for both cases. As for the case when metasurface was centered on the fetus brain, it provides the same homogeneity improvement but a bit less transmit efficiency enhancement in comparison with the dielectric pad. It may cause the fact that for this position, it was not possible to locate the metasurface close to the ROI according to the anatomical features of the voxel model. Figures 4 and 5 illustrate simulated SAR10g maps. For all cases, a decrease in SARwb was observed. Specifically, the SARwb was reduced by 1.6-fold for the cases when the entire fetus ROI was considered and by 1.8/1.2-fold (dielectric pad/metasurface) – for centering on the brain.Discussion and conclusion
The metasurface-based pad has been optimized to improve the quality of fetal MRI at 3T. Numerical simulation results have shown that a metasurface-based pad can improve the B1+ homogeneity and reduce SAR in pregnant women at the ninth month of gestation, similar to a state-of-the-art high-permittivity dielectric pad. However, the metasurface advantages are that it could be constructed from cheap making the structure ultralight and flexible. The future studies will include an investigation of the metasurface impact on pregnant women of other gestation (the third and seventh months) and experimental studies with volunteers. The authors have already received approval from the local ethic committee in Federal Almazov North-West Medical Research Center (Saint Petersburg, Russia).Acknowledgements
This work was supported by the Ministry of Education and Science of the Russian Federation (075-15-2021-592).References
1. Weisstanner C et al. Fetal MRI at 3T—ready for routine use? The British Journal of Radiology. 2016; 90:1069.
2. Collins CM et al. Central brightening due to constructive interference with, without, and despite dielectric resonance. J Magn Reson Imaging 2005; 21: 192–6.
3. De Heer et al. Increasing signal homogeneity and image quality in abdominal imaging at 3 T with very high permittivity materials. Magn Reson Med. 2012; 68(4): 1317-1324.
4. van Gemert et al. A simulation study on the effect of optimized high permittivity materials on fetal imaging at 3T. Magn Reson Med. 2019; 82(5): 1822-1831.
5. Vorobyev V et al. Improving B1+ homogeneity in abdominal imaging at 3 T with light, flexible, and compact metasurface. Magn Reson Med. 2021; DOI: 10.1002/mrm.28946.
6. Abaci Turk E et al. Individual variation in simulated fetal SAR assessed in multiple body models. Magn Reson Med. 2020;83:1418-1428.
7. International Electrotechnical Commission. IEC 60601- 2- 33: Medical electrical equipment- Particular requirements for the basic safety and essential performance of magnetic resonance equipment for medical diagnosis. https://webst ore.iec.ch/publi catio n/22705. Published 2010. Updated 2015.
Figures