2153
Feasibility of microwave ablation using two applicators with real-time MR thermometry1Radiology, Mayo Clinic, Rochester, MN, United States
Synopsis
Simultaneous use of multiple applicators is desirable in MRgMWA when treating large tumors and its feasibility is investigated in phantom experiments to evaluate the impact of MW system on MR image quality and in ex-vivo experiments with porcine tissue to compare MWA procedures with one and two applicators. Relative SNR was dropped from 88.1% with one applicator activated to 54.6% with both activated, yet temperature and tissue damage maps with acceptable image quality were obtained. Simultaneous use of two MW applicators could significantly increase the treatment efficiency with a larger ablation zone when both applicators are properly selected and configured.
Introduction
Magnetic resonance (MR)-guided microwave ablation (MRgMWA) has been demonstrated to be an effective minimally invasive treatment for a range of localized tumors. MRI guidance is advantageous as it can provide excellent contrast for tumor delineation, applicator placement, real-time treatment progress monitoring, and immediate treatment outcome prediction 1-5. MRgMWA is usually performed with a single microwave applicator, multiple rounds of ablations are thus required to sufficiently treat tumors with the maximal tumor diameter above the typical ablation diameter (~5.5 cm), resulting in extended total procedure time due to repeated applicator placement and ablation 6. Simultaneous use of multiple applicators is therefore desirable in these cases. The purpose of this work is to investigate the feasibility and effectiveness of MRgMWA using two microwave applicators simultaneously, including the impact of elevated electronic noise level and intermittent electromagnetic interference (EMI) on MR image quality, especially during real-time MR thermometry (MRT) 1, 2, 4, 5.Methods
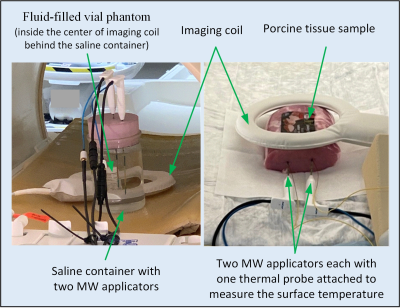
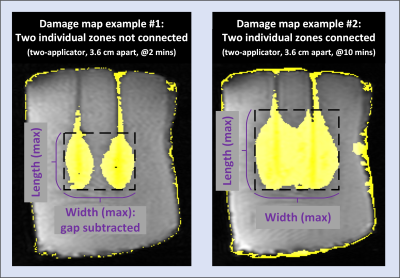
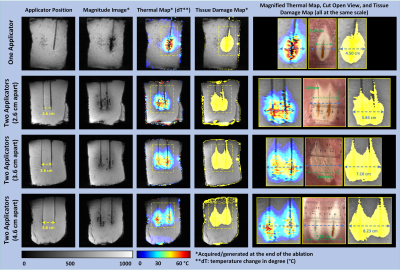
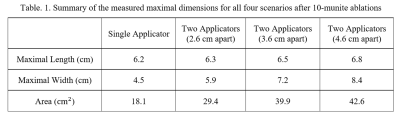
Experiments were conducted on a 1.5T MRI scanner (Ingenia, Philips, Best, Netherlands) with two MRI-configured MWA systems each including a microwave generator and a set of MRI-conditional applicators (Avecure, MedWaves Inc., San Diego, CA) 4, 5, 7. Experiments using a fluid-filled vial phantom (Figure 1 left) were first performed to evaluate the impact of MW system on MR image quality by characterizing the signal to noise ratio (SNR) under various conditions: both generators powered off (baseline), one powered off and the other activated, both in standby mode, and both activated.MWA experiments in ex-vivo porcine tissue phantoms (Figure 1 right) were then conducted for 10 minutes with one or two applicators. Each individual MWA procedure was performed in a separate phantom of fresh tissue. Two microwave applicators orientated in parallel were inserted into the tissue both at a depth of 10 cm. Three MWA experiments were performed with two applicators spaced 2.6, 3.6, and 4.6 cm apart. An additional MWA experiment was also performed with one applicator. During each ablation, MR image data were continuously collected using a 2D spoiled gradient-recalled echo sequence for MRT. K-space EMI correction was performed to suppress the intermittent EMI for improved temperature and tissue damage maps 8. The treatment zone in each damage map was characterized by its maximal width (perpendicular to the applicator shaft), maximal length (along the applicator shaft), and the treatment area in the damage map within a rectangular ROI defined by the maximal width and length (Figure 2).
Results
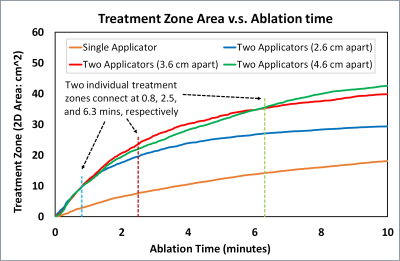
The introduction of an additional microwave system (generator and applicator) resulted in a drop of relative SNR from 88.1 ± 2.9% with one applicator activated to 54.6 ± 6.4% with both activated. Temperature and tissue damage maps with acceptable image quality were obtained, especially after EMI corrections, as demonstrated in Figure 3. Individual ablation zones generated by two applicators spaced at 2.6, 3.6, and 4.6 cm apart connected at 0.8, 2.5, and 6.3 minutes, respectively. In all experiments the length of the treatment zone along the applicator shaft was essentially the same. The ablation zone in the single applicator case had consistently smaller maximal width and area throughout the entire ablation procedure (Figure 4). The quantifications of the maximal width and area of the treatment zones for three two-applicator scenarios were time dependent. In the initial stage of the MWA (e.g., prior to 1.5 minutes), these two quantities were similar for all three two-applicator scenarios, and the scenario with 2.6 cm provided the lowest maximal width and area afterwards. The two-applicator scenario with 3.6 cm apart provided higher values than that with 4.6 cm at approximately 1.5–4.5 minutes for maximal width and 1.5–6.0 minutes for area. The one with 4.6 cm apart eventually formed the largest treatment zone at the end of the 10-minute ablation. Quantifications of all maximal dimensions were summarized in Table 1.Discussion
Compared to MWA with a single applicator, an additional ~33% drop of SNR was measured with two applicators on the MR magnitude images. K-space EMI corrections were particularly helpful for those frames acquired right after the microwave systems were activated where EMI was severe. A smaller distance between two applicators (e.g., 2.6 cm) may treat the central region sooner and more completely with more uniform coverage parallel to the applicators while a bigger distance (e.g, 4.6 cm) would create a larger treatment zone with a valley in the middle of the merged treatment zone. In addition, the total ablation duration was fixed as 10 minutes as normally used in clinical practice. In practical patient treatments, proper distance between two applicators as well as treatment duration should be determined based on tissue property, specific size, shape, and location of the target tumor(s) by the interventional radiologist.Conclusion
This work demonstrated that despite the decrease in image SNR when two microwave applicators are simultaneously applied, acceptable real-time MRT can still be obtained for MRgMWA. Simultaneous use of two MW applicators could significantly increase the treatment efficiency with a larger ablation zone, especially when distances between two applicators and treatment duration are properly selected. Evaluations of this technique on patients are underway.Acknowledgements
No acknowledgement found.References
1. Chen, J.C., et al., Prostate Cancer: MR Imaging and Thermometry during Microwave Thermal Ablation-Initial Experience. Radiology, 2000. 214(1): p. 290-297.
2. Morikawa, S., et al., MR-guided microwave thermocoagulation therapy of liver tumors: Initial clinical experiences using a 0.5 T open MR system. Journal of Magnetic Resonance Imaging, 2002. 16(5): p. 576-583.
3. Kaltenbach, B., et al., Real-time qualitative MR monitoring of microwave ablation in ex vivo livers. International Journal of Hyperthermia, 2016. 32(7): p. 757-764.
4. Gorny, K.R., et al., Practical implementation of robust MR-thermometry during clinical MR-guided microwave ablations in the liver at 1.5 T. Physica Medica, 2019. 67: p. 91-99.
5. Lu, A., et al., Improved MR-thermometry during hepatic microwave ablation by correcting for intermittent electromagnetic interference artifacts. Physica Medica, 2020. 71: p. 100-107.
6. Simon, C.J., D.E. Dupuy, and W.W. Mayo-Smith, Microwave Ablation: Principles and Applications. RadioGraphics, 2005. 25(suppl_1): p. S69-S83.
7. Ma, C., et al., Protocol for testing suitability of compact US imaging systems for use inside MRI suites, and application to one commercial US system. Biomedical Physics & Engineering Express, 2016. 2(4): p. 047003.
8. Rieke, V. and K. Butts Pauly, MR thermometry. Journal of Magnetic Resonance Imaging, 2008. 27(2): p. 376-390.
Figures