2132
Preoperative Evaluation of Potential Living Liver Donors with MRI1Radiology, University of Wisconsin-Madison, Madison, WI, United States, 2Surgery, University of Utah, Salt Lake City, Salt Lake City, UT, United States, 3University of Wisconsin-Madison, Madison, WI, United States, 4Engineering, University of Wisconsin-Madison, Madison, WI, United States, 5Medical Physics, University of Wisconsin-Madison, Madison, WI, United States, 6Medicine, University of Wisconsin-Madison, Madison, WI, United States, 7Emergency Medicine, University of Wisconsin-Madison, Madison, WI, United States
Synopsis
The growing need for liver transplantation has led to an increased need for living liver donors. Partial hepatectomy in donors carries significant risk, requiring rigorous preoperative evaluation. Contrast-enhanced MRI and MR cholangiography can assess liver lesions and biliary variants, while chemical shift-encoded MRI and MR elastography detect and quantify fat, iron and fibrosis in unexpected diffuse liver disease. This study summarizes our experience with an extended MRI protocol in 68 potential donors. MRI, in isolation or in combination with other test results identified more than half of patients at risk for surgical complications of liver donation.
INTRODUCTION
In order to meet the growing need for liver transplantation in patients with liver failure, there is an increased need for living donors. Liver donation carries significant risk to both donor and recipient. Therefore, extensive preoperative evaluation is required, including evaluation of biliary and vascular variant anatomy and the presence of unexpected diffuse liver disease. MR cholangiopancreatography (MRCP) and contrast-enhanced MR cholangiography (MRC), and MRI can be used to assess biliary anomalies and focal liver lesions. Chemical shift-encoded (CSE)-MRI and MR elastography (MRE) provide accurate quantification of fat, iron and fibrosis, in unexpected diffuse liver disease. Importantly, hepatic steatosis is an independent predictor of perioperative complications in liver resection1, as steatotic livers have poor graft function and decreased donor survival2. Furthermore, evaluation of the biliary anatomy is relevant, as biliary complications, such as bile leakage and ductal strictures, are major causes of morbidity/mortality in recipients3.T1 weighted (T1w) MRC and MRI using gadoxetic acid (Bayer Healthcare Pharmaceutical, Wayne, NJ), a hepatocyte specific contrast agent with dual excretion (renal and biliary), are valuable for identification of biliary variants4,5, and the detection and characterization of liver lesions6.
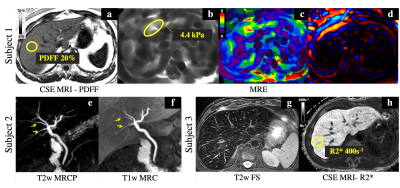
In order to evaluate for the presence of unexpected diffuse liver disease, CSE-MRI provides proton density fat fraction (PDFF, expressed in %)7, a biomarker of hepatic steatosis8,9, and also R2*, a biomarker of liver iron overload10. MRE assesses stiffness of liver tissue as an established biomarker of presence of liver fibrosis.
The purpose of this study was to summarize our clinical experience with an extended MRI protocol in potential living liver donors, and demonstrate the relevance of MRI in the management of liver donors.
METHODS
This retrospective study was performed with Institutional Review Board approval, including a waiver of informed consent. Electronic health records (EHR) were searched for all MRI examinations performed between January 1, 2017 and July 30, 2020 in potential living liver donors at our institution.Work-up for live liver donation
Medical screening tests for potential liver donors at our institution typically include, but are not limited to: history and physical exam; abdominal MRI and CT angiography (CTA); chest X-ray; mammogram (in women); cardiac testing; extensive blood work, and; consultation with living donation team including hepatologist, surgeon, psychologist and others.
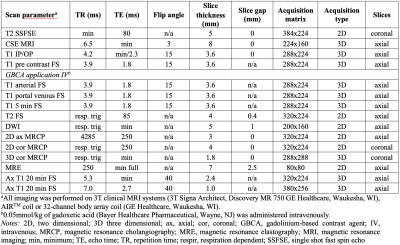
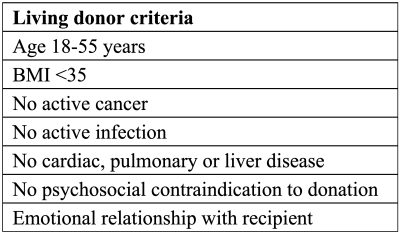
The details of an extended MRI protocol, including MRCP, T1w gadoxetic acid-enhanced MRC and MRI, CSE-MRI and MRE, are shown in Table 1. Criteria for live liver donation are shown in Table 2.
Data collection
The following clinical data were collected from the EHR: demographics, MRI and other imaging reports; laboratory findings; information regarding peri- or postoperative complications (if any). The decision process for potential living liver donation was reviewed in detail by a radiologist and surgeon, by consensus.
All MRI examinations were initially interpreted by experienced fellowship trained abdominal radiology faculty, and formally reviewed by a radiologist with 9 years of experience in abdominal imaging to tabulate abnormal MRI findings.
Statistical analysis was performed using Excel (v16.30, Microsoft, Washington).
RESULTS
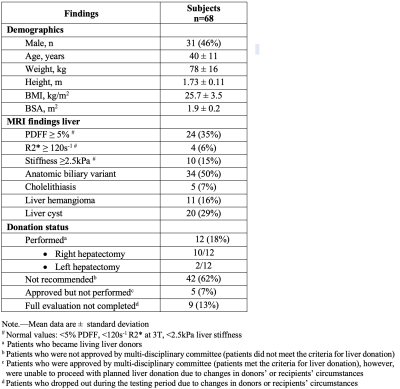
68 gadoxetic acid-enhanced MRI examinations were performed in 68 potential living liver donors (male 46%; Table 3) on a clinical 3.0T MRI systems (GE Healthcare, Waukesha, WI, Table 1). In 4 patients, MRE was not performed, and in 9 patients MRE was considered non-diagnostic.MRI revealed hepatic steatosis (≥5% PDFF) in 24/68 (35%) subjects including: 11 subjects with PDFF 5-9%, 8 with PDFF 10-14%, and 5 with PDFF >15%. 4/68 (6%) subjects had elevated liver iron (R2*≥120s-1, Table 3) with R2* values of 130s-1, 150s-1, 260s-1and 400s-1. MRE results found 8 patients with mildly elevated liver stiffness indicating possible liver inflammation (2.5-2.9 kPa), 1 patient with stage 2-3 fibrosis (3.6-4.0 kPa) and 1 patient with stage 3-4 fibrosis (4.1-5.0 kPa).
Biliary variants were found in 34/68 (50%) of subjects, and 38/68 (50%) had other incidental findings, including liver hemangioma, liver cysts and cholelithiasis (Table 3).
As part of a multi-disciplinary conference review, living liver donation was approved in 17/68 (25%) donor candidates, although executed in only 12/68 (18%, Table 3). 9/68 of subjects dropped out from the donation program during testing due to changes in donors’ or recipients’ circumstances. 42/68 (62%) of subjects were not recommended for liver donation based on examination findings. Results of MRI alone, or in combination with results of other tests, led to 22/42 (52%) of all rejections (Figure 1, 2).
DISCUSSION
In this work we have described our clinical experience with an extended MRI protocol for evaluation of liver in potential living liver donors. This work demonstrates that MRI plays a major role in selection and management of live liver donors. MRI not only identified focal liver lesions, but also identified anatomic biliary variants, detected abnormally elevated liver fat, iron and stiffness. Importantly, MRI, in isolation or in combination with other test results identified more than half of patients at risk for surgical complications of liver donation.CONCLUSION
In conclusion, MRI plays a major role in the acceptance or rejection of potential living liver donors.Acknowledgements
The authors wish to acknowledge support from GE Healthcare and Bracco Diagnostic who provide research support to the University of Wisconsin. Dr. Reeder is a Romnes Faculty Fellow, and has received an award granted by the University of Wisconsin-Madison Office of the Vice Chancellor for Research and Graduate Education with funding from the Wisconsin Alumni Research Foundation.References
- Kooby D. Impact of steatosis on perioperative outcome following hepatic resection. Journal of Gastrointestinal Surgery. 2003;7(8):1034-1044. doi:10.1016/j.gassur.2003.09.0122.
- Chu MJJ, Dare AJ, Phillips ARJ, Bartlett ASJR. Donor Hepatic Steatosis and Outcome After Liver Transplantation: a Systematic Review. J Gastrointest Surg. 2015;19(9):1713-1724. doi:10.1007/s11605-015-2832-13.
- Kim B, Kim SY, Kim KW, et al. MRI in donor candidates for living donor liver transplant: Technical and practical considerations: Living Donor Liver Transplant. J Magn Reson Imaging. 2018;48(6):1453-1467. doi:10.1002/jmri.262574.
- Kinner S, Schubert TB, Said A, Mezrich JD, Reeder SB. Added value of gadoxetic acid-enhanced T1-weighted magnetic resonance cholangiography for the diagnosis of post-transplant biliary complications. Eur Radiol. 2017;27(10):4415-4425. doi:10.1007/s00330-017-4797-95.
- Frydrychowicz A, Lubner MG, Brown JJ, et al. Hepatobiliary MR imaging with gadolinium-based contrast agents. J Magn Reson Imaging. 2012;35(3):492-511. doi:10.1002/jmri.228336.
- Bormann RL, Rocha EL da, Kierzenbaum ML, Pedrassa BC, Torres LR, D’Ippolito G. The role of gadoxetic acid as a paramagnetic contrast medium in the characterization and detection of focal liver lesions: a review. Radiol Bras. 2015;48(1):43-51. doi:10.1590/0100-3984.2013.17947.
- Reeder SB, Hu HH, Sirlin CB. Proton density fat-fraction: A standardized mr-based biomarker of tissue fat concentration. J Magn Reson Imaging. 2012;36(5):1011-1014. doi:10.1002/jmri.237418.
- Yokoo T, Serai SD, Pirasteh A, et al. Linearity, Bias, and Precision of Hepatic Proton Density Fat Fraction Measurements by Using MR Imaging: A Meta-Analysis. Radiology. 2018;286(2):486-498. doi:10.1148/radiol.20171705509.
- Starekova J, Hernando D, Pickhardt PJ, Reeder SB. Quantification of Liver Fat Content with CT and MRI: State of the Art (Publication in Press). Radiology. Published online 2021.10.
- Hernando D, Levin YS, Sirlin CB, Reeder SB. Quantification of liver iron with MRI: State of the art and remaining challenges: Liver Iron Quantification Using MRI. J Magn Reson Imaging. 2014;40(5):1003-1021. doi:10.1002/jmri.24584
Figures
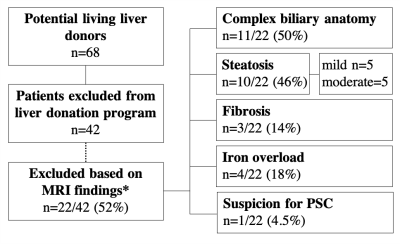
Figure 1: MRI Role in decision making for living liver donation. Listed are MRI findings in subjects excluded from the live liver donation.
*MRI findings alone or in combination with other findings (laboratory, imaging, psychosocial aspects) were the reason for exclusion from living liver program in 22/42 (52%) cases. Notes: n, number; PSC, primary sclerosing cholangitis