2130
Feasbility of 3D MRCP for patients in both supine and prone position: a comparison study of qualitative and quantitative assessment1Renmin Hospital of Wuhan University, wu han, China, 2GE Healthcare, Beijing, China
Synopsis
Increasing evidence has suggested that endoscopic retrograde cholangiopancreatography (ERCP) in the supine position is technically more technically demanding for operators than prone ERCP and leads to a greater risk of adverse cardiorespiratory events. Our results showed no differences in the CR, SNR, and CNR of the CBD between MRCP image sets. The visibility of most pancreaticobiliary ducts, motion artifact, and overall image quality were slightly better on the prone MRCP images than on the supine ones (P < 0.005). Therefore, 3D prone MRCP could provide better visualization and a roadmap directly matched with prone ERCPs for clinicians performing a surgery.
Introduction
Magnetic resonance cholangiopancreatography (MRCP) is a noninvasive and contrast-free imaging technique. It can exquisitely depict the biliary tree anatomy and pancreatic duct with excellent spatial resolution and image quality as a roadmap for gastroenterologists who are preparing for surgery. Clinically, ERCP is most commonly used in the removal of bile duct stones and relief of malignant obstructive jaundice and sets up in a supine and prone position, respectively, for the purpose of pre-operation and operation exam. Increasing evidence has suggested that ERCP in the supine position is technically more technically demanding for and leads to a greater risk of adverse cardiorespiratory events. Therefore, the purpose of this study was to evaluate the clinical feasibility of 3D MRCP in both supine and prone position via quantitative and qualitative assessment.Methods
We recruited seventy-eight consecutive patients from department of gastroenterology who need MRCP between August 2021 and October 2021. Eligible patients complete respiratory-triggered fat-suppressed MRCP in both prone and supine position with the same scan parameters on a 3.0T MR scanner (Signa Discovery 750w, GE Healthcare, Milwaukee, USA) using an 18-channel body matrix coil combined with a 32-channel spine matrix coil. Patients should be fasting for approximately 4-6 hours prior to the MRCP to ensure gallbladder filling and gastric emptying. No spasmolytic drug or negative oral contrast was used. All images were anonymized and randomly divided into two groups. Two radiologists respectively with 5 and 12 years of MRCP experience were blind to group and patient position and performed image analysis. Three slices, upper, middle, and lower common bile duct (CBD), relative to the center of CBD in each patient were chosen. Signal intensity (SI) was measured by placing circular regions of interest (ROIs) on the CBD and periductal tissues . The signal-to-noise ratio (SNR = SICBD/SDCBD), contrast ratio [CR = (SICBD − SIperiductal tissue)/(SICBD+ SIperiductal tissue)], contrast to noise ratio [CNR = (SICBD – SIperiductal tissue)/ SDCBD] were calculated. In addition, image quality was evaluated with a 5-point Likert-type scale including artifacts, background suppression, overall image quality, and ductal visualization.The interobserver agreement was evaluated by Cohen’s κ values (fair: 0.21–0.40, moderate: 0.41–0.60, good: 0.61–0.80, excellent: 0.81–1.00). A paired t-test or Wilcoxon signed-rank test depending on data normality was used to compare the area of bile duct, SNR, CR,CNR, artifacts, overall imaging quality, ductal visualizationbetween 3D MRCP in the supine and prone position. Statistical analysis was performed using SPSS 26.0 software (IBM Corp, Armonk, NY). P value <0.05 was considered statistically significant.
Results
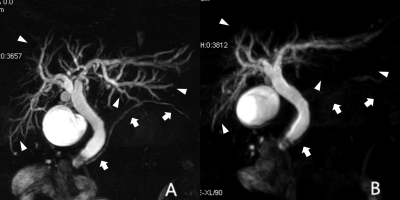
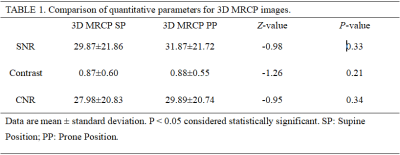
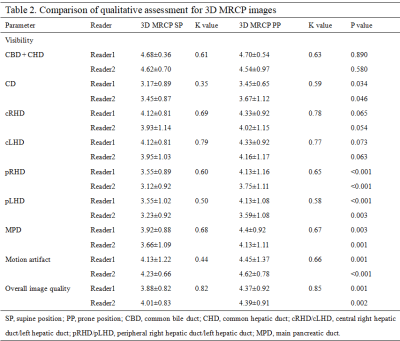
All MRCP studies were completed successfully. Objective assessment was summarized in Table 1. SNR,CR and CNR of the CBD were slightly higher on 3D MRCP-PP than those on 3D MRCP-SP (31.87±21.72 vs 29.87±21.86, P=0.33; 0.88±0.55 vs 0.87±0.60, P = 0.21; 29.89±20.74 vs 27.98±20.83, P = 0.34), respectively. However, there was no statistically significant differences between the 3D MRCP in the prone and supine examinations. The qualitative assessment of pancreaticobiliary ducts, motion artifact and overall image quality are summarized in Table 2. The qualitative scores of the cystic duct (CD), peripheral right hepatic duct (pRHD), peripheral left hepatic duct (pLHD), main pancreatic duct(MPD) were significantly higher on 3D MRCP-PP than 3D MRCP-SP by readers 1 and 2 (P < 0.001– 0.046) (Fig. 1).The Cohen’s value in presentation of the interobserver agreement for the visibility of all pancreaticobiliary ducts were 0.58–0.85 on 3D MRCP-PP and 0.35–0.82 on 3D MRCP-SP.Discussion
This was the first study to compare 3D MRCP images of the same patients in both supine and prone position. Our results showed that 3D MRCP in the prone position offered better visualization of pancreaticobiliary ducts but equivalently good display of part of pancreaticobiliary ducts on that 3D supine MRCP images. According to anatomical geography of body organs, the liver is located above the second portion of the duodenum when the patient is in the supine position and thus the bile flows into the small intestine due to gravity. When the patient is in the prone position, the liver is located under the duodenum and thus bile flows under anti-gravity conditions, filling the small ducts. Therefore, this might explain for better visualization of small ducts on 3D prone MRCP, providing a roadmap directly matched with prone ERCPs for clinicians performing a surgery.Acknowledgements
No acknowledgement found.References
1.Kromrey Marie-Luise,Funayama Satoshi,Tamada Daiki et al. Clinical Evaluation of Respiratory-triggered 3D MRCP with Navigator Echoes Compared to Breath-hold Acquisition Using Compressed Sensing and/or Parallel Imaging.[J] .Magn Reson Med Sci, 2020, 19: 318-323.
2.Chen Zhiyong,Sun Bin,Xue Yunjing et al. Comparing compressed sensing breath-hold 3D MR cholangiopancreatography with two parallel imaging MRCP strategies in main pancreatic duct and common bile duct.[J] .Eur J Radiol, 2021, 142: 109833.
Figures