2046
Characterization of Symptomatic Vertebrobasilar Plaques in Diabetic Patients Using Computed Tomographic Angiography and Vessel Wall Imaging1Radiology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China, 2Radiology, Qilu Hospital of Shandong University, Jinan, China, 3Geriatric Neurology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China, 4MSC Clinical & Technical Solutions, Philips Healthcare, Beijing, China
Synopsis
Diabetes mellitus is significantly associated with posterior circulation ischemic stroke. We aimed to compare the characteristics of vertebrobasilar plaques in symptomatic patients with and without diabetes using vessel wall magnetic resonance imaging and computed tomographic angiography. Characteristics of symptomatic vertebrobasilar plaques were compared between patients with and without diabetes. Multivariate analysis demonstrated differences in the presence of T1 hyperintensity and number of spotty calcifications were statistically significant. Symptomatic patients with diabetes have a higher incidence of T1 hyperintensity and larger calcification burden than those without diabetes, indicating the association of diabetes with more advanced plaque features in the posterior circulation.
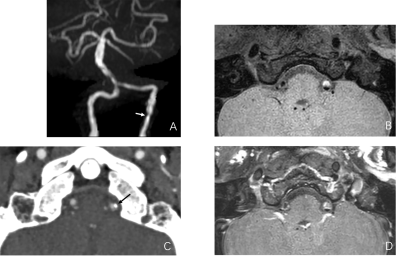
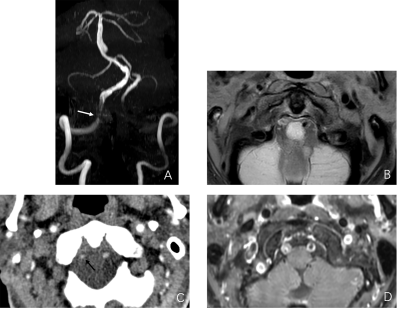
Methods: From April 2017 to June 2021, all patients who underwent both HR-VWI and CTA were retrospectively reviewed. The inclusion criteria were (1) presence of transient ischemic attack or stroke in the territory of posterior circulation; (2) HR-VWI and CTA examinations within a time interval of 4 weeks after the onset of neurological symptoms. DM patients were divided into 2 subgroups by the level of glycated hemoglobin (HbA1c) (≥7.0% as high-HbA1c group vs. <7.0% as low-HbA1c group) and diabetes duration (shorter [ 0-9 years] vs. longer [>10 years]). All MRI and MRA exams were performed on a 3T MR imaging scanner (Ingenia; Philips Healthcare) with a 16-channel head coil. The standardized imaging protocol included DWI, time-of-flight magnetic resonance angiography or phase-contrast magnetic resonance angiography, pre-and post-contrast T1-weighted HR-VWI. The HR-VWI sequence was performed using a volumetric isotropic turbo spin-echo acquisition (VISTA; Philips Healthcare) in coronal and axial planes for comprehensive intracranial artery coverage and optimal blood suppression. The following parameters were used: TR/TE, 425ms/19ms; field of view, 220×220 mm; matrix, 316×312; TSE factor, 28 including 2 startup echoes; oversampling factor, 1.3; number of average, 2; SENSE factor, 2; echo spacing, 6.3 ms; acquired resolution, 0.7×0.7×1.1 mm3; and scan time, 6.1 minutes. Plaque morphological measurements included lumen area, outer wall area, normal wall index, maximum wall thickness, minimum wall thickness, eccentricity index and remodeling index. Signal characteristics including plaque enhancement and T1 hyperintensity were analyzed based on the previous criteria(3, 4). CTA protocol was conducted on a 128-slice dual-source CT scanner (SOMATOM Definition Flash, Siemens healthiness, Forchheim, Germany). Same reconstruction parameters were used for single phase CTA and 4D multi-phase CTA (a section thickness of 1.0 mm; an interval of 0.7 mm). Calcification was defined as the presence of hyperdensity with a CT attenuation of 130 HU or greater. Spotty calcification was defined as a lesion of calcium deposition with a length below 3 mm and within an arc of less than 90°. The calcification volume was quantified semiautomatically using Medical Imaging Interaction Toolkit (MITK, open-source software, https://www.mitk.org).
Results: A total of 148 patients were included and 75 patients were diagnosed with diabetes mellitus. DM patients were more likely to have a history of prior stroke (49% vs. 33%, p=0.034) compared to non-DM patients. Diabetic patients had more presence of T1 hyperintensity, calcification and spotty calcification, as well as higher calcification volume (all p<0.05) compared with non-diabetic patients. Multivariable logistic regression model demonstrated that the associations of T1 hyperintensity (OR, 2.40 [95% CI, 1.03 to 5.77], p=0.045) and number of spotty calcifications (β, 0.37 [95% CI, 0.01 to 0.73], p=0.047) with the presence of DM were statistically significant after adjusting for baseline characteristics. Compared with patients with the low-HbA1c level, patients with the high-HbA1c level demonstrated significantly more presence of T1 hyperintensity (44% vs. 20%, p=0.047).
Conclusion: Symptomatic diabetic patients have a higher incidence of T1 hyperintensity and larger calcification burden than those without diabetes mellitus, indicating that diabetic patients may be associated with more advanced plaque features in the posterior circulation.
Discussion: In the present study, DM patients demonstrated a higher prevalence of T1 hyperintensity and spotty calcification presence and larger calcification burden than non-DM patients in the vertebrobasilar artery. Culprit plaques in diabetics demonstrated more presence of spotty calcification than those in non-diabetics, with an expected increase number of 0.37 per plaque. Hyperglycemia could accelerate inflammation and oxidative stress, promoting plaque calcification in both intima and media(5). Spotty calcification could represent an active state of the dynamic process of atherosclerosis. Overall, the number of spotty calcifications in the vertebrobasilar artery was relatively paucity, in agreement with the recent case-control study by Zhao et al(6). As a recognized high-risk plaque feature, IPH originates from the disruption of incomplete neovessels, aggravated by inflammation. Our study was in consistent with the pathologic observations reported increased neovascularization and IPH grade in diabetic plaques(7). The diabetic-specific features of plaque vulnerability may indicate the association between DM and its preference for posterior circulation ischemic stroke.
Acknowledgements
This work was supported by the Natural Science Foundation of Shandong Province (grant no.ZR2018BH029, ZR2020QH266), National Natural Science Foundation of China (grant no.82000771), and Academic Promotion Programme of Shandong First Medical University (no.2019QL023).References
1. Luitse MJ, Biessels GJ, Rutten GE, et al. Diabetes, hyperglycaemia, and acute ischaemic stroke. Lancet Neurol. 2012;11(3):261-71.
2. Moreno PR, Fuster V. New aspects in the pathogenesis of diabetic atherothrombosis. J Am Coll Cardiol. 2004;44(12):2293-300.
3. Xu WH, Li ML, Gao S, et al. Middle cerebral artery intraplaque hemorrhage: prevalence and clinical relevance. Ann Neurol. 2012;71(2):195-8.
4. Yang H, Ji C, Wang H, et al. Characterisation of symptomatic intracranial plaque without substantial stenosis using high-resolution vessel wall MRI. Clin Radiol. 2021;76(5):392 e21- e26.
5. Yahagi K, Kolodgie FD, Lutter C, et al. Pathology of Human Coronary and Carotid Artery Atherosclerosis and Vascular Calcification in Diabetes Mellitus. Arterioscler Thromb Vasc Biol. 2017;37(2):191-204.
6. Zhang F, Yang L, Gan L, et al. Spotty Calcium on Cervicocerebral Computed Tomography Angiography Associates With Increased Risk of Ischemic Stroke. Stroke. 2019;50(4):859-66.
7. Purushothaman KR, Purushothaman M, Muntner P, et al. Inflammation, neovascularization and intra-plaque hemorrhage are associated with increased reparative collagen content: implication for plaque progression in diabetic atherosclerosis. Vasc Med. 2011;16(2):103-8.
Figures