2033
Value of high b-value computed diffusion-weighted imaging in intraductal papillary mucinous neoplasia of the pancreas1Institute of Diagnostic and Interventional Radiology, Technical University of Munich, School of Medicine, Munich, Germany, 2Philips GmbH Market DACH, Hamburg, Germany, 3Department of Surgery, Technical University of Munich, School of Medicine, Munich, Germany, 4Department of Medicine II, Technical University of Munich, School of Medicine, Munich, Germany
Synopsis
The incidence of intraductal papillary mucinous neoplasms (IPMN), which represent a potential precursor of pancreatic cancer, is increasing. We herein investigate the potential of computed high b-value diffusion-weighted imaging (cDWI) in detection and stratification of IPMN. cDWI at b = 1000 s/mm2 increases lesion detection rates as well as diagnostic sensitivity and specificity regarding the presence of malignant imaging features. Combining cDWI and high-resolution reduced field-of-view imaging further increases diagnostic accuracy. cDWI seems particularly promising in view of the need for non-invasive lesion detection and characterization due to the recent paradigm shift from surgery to active surveillance of IPMN.
Introduction
Advances in high-resolution cross-sectional imaging have led to an increased discovery rate and thus incidence of cystic pancreatic lesions, such as intraductal papillary mucinous neoplasms (IPMN)1. IPMN stem from the mucinous epithelium of the pancreatic duct and represent precancerous lesions, potentially progressing to pancreatic cancer. IPMN treatment ranges from surveillance to surgical resection, depending on their malignant potential, estimated from imaging features, clinical symptoms and laboratory values. Previous studies propagated the added value of diffusion-weighted imaging (DWI) in differentiating between benign and malignant IPMN using b-values up to 800 s/mm2 2. Moreover, b-values of b ≥ 1000s /mm2 have been reported to add diagnostic value in DWI of pancreatic cancer3. Yet, the application of high b-value DWI is restricted in clinical routine since longer acquisition lead to patient discomfort, limited patient throughput and compromised image quality due to motion. Artificially generated computed high b-value DWI (cDWI) have been proposed as a means to overcome these limitations4. Furthermore, high-resolution reduced field-of-view DWI (rFOV-DWI) improves both image quality and lesion delineation in pancreatic pathologies5. We herein investigate the diagnostic value of high b-value cDWI and the added value of high-resolution high b-value cDWI in IPMN of the pancreas.Methods
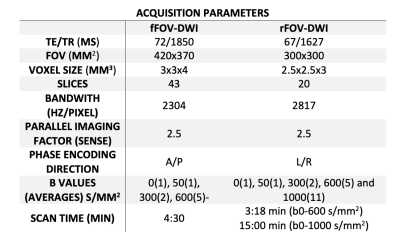
88 patients (71±10 years, 53 female, 35 male) with a diagnosis of IPMN were retrospectively enrolled. In all patients, a 2D diffusion-weighted (DW) single-shot echo planar imaging (ssEPI) sequence with full field-of-view (fFOV) for full upper abdomen coverage was acquired at the following b-values (averages): 0(1), 50(1), 300(2), 600(5) s/mm2. In a subset of 39 patients, an additional 2D DW ss-EPI sequence with reduced field-of-view (rFOV) for high-resolution pancreatic imaging was performed at the same b values as in the fFOV cohort. Furthermore, in a subset of 21 patients with rFOV-DWI an additional high b value at b = 1000 (11) s/mm2 was acquired (r-aDWI1000). Images were acquired at 3T. Detailed sequence parameters are displayed in Table 1. Using dedicated software, cDWI datasets at b = 1000 s/mm2 were calculated from b = 0, 50, 300 and 600 s/mm2 datasets based on a mono-exponential fit model for fFOV (f-cDWI1000) and rFOV (r-cDWI1000), respectively. Following qualitative image parameters were rated on a 4-point Likert scale (1=worst, 4=best) by two experienced radiologists: Image quality, lesion detection/delineation, fluid suppression within the lesion. The contrast ratio between the lesion and the adjacent normal parenchyma was calculated as follows: CR = SI lesion / SI normal pancreas.Diagnostic confidence regarding the presence/absence of diffusion restricted nodules/masses was rated on a 4-point Likert scale (4 = definitely nodule/mass, 3 = probably nodule/mass, 2 = probably no nodule/mass 1 = no nodule/mass) in a subgroup of 68 patients. Endoscopic ultrasound and postoperative pathological report served as the standard of reference.
Results
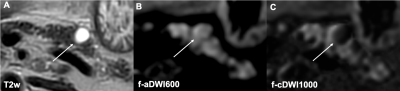
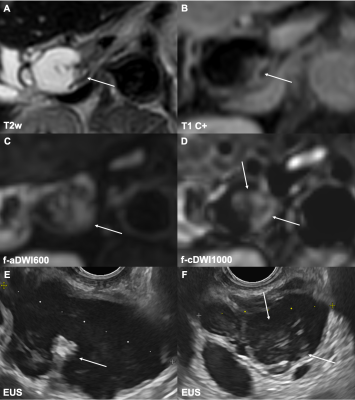
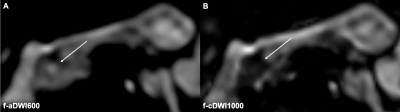
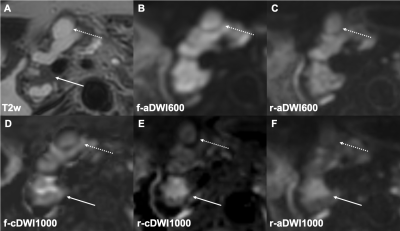
Image quality was rated higher in acquired datasets at b = 600 s/mm2, compared to computed datasets at b = 1000 s/mm2, holding true for both fFOV- and rFOV-DWI (p = 0.001, p < 0.001). Comparing both computed datasets revealed higher image quality in r-cDWI1000 (p < 0.001) compared to f-cDWI1000. No significant difference was found between r-aDWI1000 and r-cDWI1000 datasets (p = 0.083). Lesion detection and fluid suppression were rated in favor of both computed b = 1000 s/mm2 datasets compared to acquired datasets at b = 6000 s/mm2 (p < 0.001) (Fig. 1,). r-cDWI1000 outperformed f-cDWI1000 (p < 0.001) and no difference was found between r-aDWI1000 and r-cDWI1000 (p = 0.206). CR was significantly higher in both computed datasets at b = 1000 s/mm2 compared to acquired datasets at b = 600 s/mm2 (p = 0.00012-0.01174). Regarding diagnostic accuracy, f-aDWI600 achieved a sensitivity, specificity and ROC of 0.33, 0.78 and 0.55 whereas sensitivity, specificity and ROC were 0.78, 0.96 and 0.89 in f-cDWI1000 datasets; p < 0.0001 (Fig. 2, 3).The same finding was seen in high-resolution rFOV-DWI datasets. r-aDWI600 received a sensitivity, specificity and ROC of 0.50, 0.74 and 0.59, whereas sensitivity, specificity and ROC were 0.88, 0.96 and 0.91 in r-cDWI1000 datasets; p = 0.003. ROC did not differ between r-aDWI1000 and r-cDWI1000; p = 0.27 (Fig. 4).Discussion
Our study is, to our knowledge the first to evaluate the diagnostic impact of high b-value cDWI in the diagnostic work-up of IPMN. cDWI at b = 1000 s/mm2 significantly improved lesion detection/delineation and fluid suppression compared to acquired datasets at b = 600 s/mm2. Furthermore, high-resolution rFOV-DWI outperformed conventional fFOV-DWI in computed datasets. Moreover, f-cDWI1000 and r-cDWI1000 significantly improved diagnostic sensitivity and specificity regarding the presence of mural nodules, which represent a high-risk feature in IPMNs. Also, computed rFOV datasets were non-inferior to directly acquired datasets at b = 1000 s/mm2. Reduced image quality found in cDWI can be attributed to misregistration artifacts resulting from misalignement between the acquired low b-value images. Advanced image registration tools could help to overcome this issue6.Conclusion
Our study underlines the potential clinical significance of high b-value cDWI, also in combination with high-resolution rFOV-DWI, in imaging of pancreatic IPMN. Our results seem particularly interesting in light of the rising incidence of IPMN in synopsis with now stricter indications for surgical resection, thus demanding a more prominent position of non-invasive screening modalities, such as MRI.Acknowledgements
Kilian Weiss is an employee of Philips.References
1. M.L. Kromrey, R. Bülow, J. Hübner, C. Paperlein, M.M. Lerch, T. Ittermann, H. Völzke, J. Mayerle, J.P. Kühn, Prospective study on the incidence, prevalence and 5-year pancreatic-related mortality of pancreatic cysts in a population-based study, Gut 67(1) (2018) 138-145.
2. K.M. Jang, S.H. Kim, J.H. Min, S.J. Lee, T.W. Kang, S. Lim, D. Choi, Value of diffusion-weighted MRI for differentiating malignant from benign intraductal papillary mucinous neoplasms of the pancreas, AJR. American journal of roentgenology 203(5) (2014) 992-1000.
3. Y. Fukukura, Y. Kumagae, H. Hakamada, T. Shindo, K. Takumi, K. Kamimura, M. Nakajo, A. Umanodan, T. Yoshiura, Computed diffusion-weighted MR imaging for visualization of pancreatic adenocarcinoma: Comparison with acquired diffusion-weighted imaging, European journal of radiology 95 (2017) 39-45.
4. M.D. Blackledge, M.O. Leach, D.J. Collins, D.M. Koh, Computed diffusion-weighted MR imaging may improve tumor detection, Radiology 261(2) (2011) 573-81.
5. F.N. Harder, O. Kamal, G.A. Kaissis, I. Heid, F.K. Lohöfer, S. McTavish, A.T. Van, C. Katemann, J.M. Peeters, D.C. Karampinos, M.R. Makowski, R.F. Braren, Qualitative and Quantitative Comparison of Respiratory Triggered Reduced Field-of-View (FOV) Versus Full FOV Diffusion Weighted Imaging (DWI) in Pancreatic Pathologies, Academic radiology (2020).
6. M. Akagi, Y. Nakamura, T. Higaki, Y. Matsubara, H. Terada, Y. Honda, F. Tatsugami, Y. Baba, M. Iida, K. Awai, Preliminary Results of High-Precision Computed Diffusion Weighted Imaging for the Diagnosis of Hepatocellular Carcinoma at 3 Tesla, Journal of computer assisted tomography 42(3) (2018) 373-379.
Figures